Healthcare professionals’ use of mobile phones and the internet in clinical practice
Nicole Koehler1, Olga Vujovic2, Christine McMenamin3
1Assessment and Learning Design, Deakin Learning Futures, Deakin University, Burwood Campus, Victoria, Australia 2Department of Infectious Diseases, Alfred Hospital, Victoria, Australia 3Faculty of Medicine, Nursing & Health Sciences, Monash University, Victoria, Australia
Corresponding Author: nicole.koehler@deakin.edu.au
Background: Over the last few years mobile phone applications have been designed for healthcare professionals. However, little is known in regards to healthcare professionals’ use of and attitudes towards using smartphones (and applications) within clinical practice. Thus the aims of the present study were to enumerate the number of healthcare professionals that use mobile phones within clinical practice and their attitudes towards using them. Furthermore, given that the internet preceded smartphones, we also established healthcare professionals’ attitudes towards internet use in clinical practice as a comparison.
Method: Forty-three healthcare professionals from a range of disciplines and specialities who were predominantly working in Australia completed an anonymous online survey.
Results: Ninety-one per cent of healthcare professionals owned a mobile phone of which 87% used it during clinical practice. No healthcare professional was supplied with a smartphone by their clinical/healthcare workplace. Consequently they used their privately owned device. For ten out of eleven analogous statements healthcare professionals had significantly more positive attitudes towards internet than mobile phone use in clinical practice. However, attitudes for eight of the ten statements pertaining to mobile phone use were positive. Mobile phones were perceived negatively in regard to confidentiality. Furthermore, healthcare professionals’ also had the perception that patients may think that they are using their mobile for non-medical purposes.
Conclusion: Mobiles, including smartphones, are commonly used within clinical practice and at present most healthcare professionals use their privately owned device. Despite healthcare professionals having more positive attitudes toward internet use, their attitudes towards mobile use were largely positive. Our results suggest that mobile phone use, in particular smartphone use, within clinical practice is likely to increase in the future.
Introduction
The end of the last century saw the introduction of the internet, which was rapidly taken up by individuals such that 79% of Australian households had internet access by 2010-20111. The arrival of the internet was followed by another technological invention, the smartphone. Smartphones are powerful devices that combine the conventional functions of a mobile phone with advanced computing capabilities enabling users to access software applications (commonly termed “apps”)2,3. There are currently more than 10,000 apps within the Apple App Store’s “medical, health care & fitness” category alone4. Some of these apps are specifically designed for healthcare professionals such as medical calculators5,6, logbooks5, medical reference tools7, medical guidelines such as resuscitation algorithms5, and drug guidelines6. The use of apps, as well as other functions smartphones enable such as viewing patients’ radiological images8,9, and communicating with colleagues10, permit healthcare professionals to perform numerous tasks at point-of-care.
Despite the great variety of apps available for different tasks, they all have one common aim, which is to assist in clinical practice to improve patient outcomes. Thus a few studies have evaluated the efficacy of some apps11-15. For example, Flannigan and McAloon found that drug dosage calculator apps increases doctors’ and medical students’ accuracy and confidence in regards to drug dosage calculations11, whereas Low et al. found that a specifically designed app improves healthcare professionals’ performance in a simulated cardiac arrest emergency scenario13. On the contrary, Zanner et al. found that non-medically trained individuals’ performance of cardiopulmonary resuscitation in a hypothetical emergency scenario was slower in those using a specifically designed app compared to those without the app14. Furthermore, the use of a specifically designed app also impeded healthcare professionals in regards to their speed at assessing an ischemic stroke12. Thus apps need to be rigorously evaluated prior to implementation within clinical practice or as a first aid tool for the general public.
Although some medical apps appear to be promising in regards to assisting healthcare professionals to provide adequate patient care, the use of mobiles within clinical practice does not come without concerns. One such concern that has been raised is the risk of pathogen transfer3,12,15. It can be argued that mobiles should be treated like all medical equipment (e.g., stethoscopes) in terms of cleaning them. However, using the same disinfectants to those used to wipe down standard medical equipment may damage mobiles3. Placing a protective cover over mobiles that can withstand the usual disinfectants used on medical equipment has been suggested but this would only be suitable for touch screen devices and not mobiles with a built in keyboard3,15.
Smartphones interfering with medical equipment, especially in critical care settings, is another concern16. One study found that smartphones placed within 3 cm of critical care equipment produced interference16. However, this problem can be overcome by ensuring that smartphones are kept at a safe distance of one metre from a critical care bed16.
Another concern associated with using smartphones within clinical practice is in regards to treating patient information in a secure manner and that this may be breached should a smartphone be lost or stolen2,17. However, these issues can be overcome if data is stored within programs that can be erased remotely when a smartphone is reported to be lost or stolen17. Closely related to this topic is that patient confidentiality could be breached when smartphones are used to send messages or images pertaining to patients3,18. Another issue of concern is whether privately owned mobiles should be used for clinical purposes (e.g., taking photographs of patients’ wounds) given that these devices are also used privately. Unless patient information can be securely separated from non-work information and erased remotely there is a concern in regards to keeping patient information confidential.
Despite the availability of thousands of medical apps4, efficacy data regarding some apps11,13, and the awareness of potential concerns associated with using smartphones in clinical practice2,3,12,15-17, there is little known in regards to healthcare professionals’ use of and attitudes towards using smartphones in clinical practice. Low et al. found that after using an app in a simulated emergency resuscitation scenario, participants did not think that using such an app is a reflection of poor training or that it appears unprofessional13. However, it must be kept in mind that Low et al.’s study involved a simulated environment, as opposed to real clinical situations, and did not obtain extensive information pertaining to healthcare professionals’ attitudes towards using mobiles in clinical practice13.
The aim of the present study was to enumerate the number of healthcare professionals that use mobiles/smartphones and apps during clinical practice. In regards to the issue of confidentiality we were particularly interested in establishing who owns the mobile used during clinical practice and the purposes it is used for (e.g., taking photographs of patients’ wounds). Given that the use of mobiles, and in particularly apps, is relatively recent we were also interested in healthcare professionals’ attitudes towards using mobiles within clinical practice. Furthermore, as a comparison, we were also interested in healthcare professionals’ attitudes towards internet use in clinical practice given that it preceded the use of apps and thus may be perceived to be more acceptable to use.
Method
Participants
Monash University staff members were invited to participate in an on-line survey on the use of mobile phones and the internet in clinical practice via an advertisement on Monash Notices (a weekly electronic university newsletter) over a 3 month period. Recruitment advertisements were also sent to 71 healthcare facilities throughout Australia. However, it is unknown as to whether these advertisements were displayed. Individuals that had obtained a healthcare qualification and had practiced within the last two years were eligible to participate.
Procedure
Ethics approval was obtained from Monash University’s Human Research Ethics Committee. The survey was created using Qualtrics (an online platform to administer surveys and collect responses). Participants were directed to the anonymous survey via a link within the recruitment advertisement.
The first two survey questions established whether participants have a healthcare qualification and whether they had practiced within the last two years. The survey terminated for participants that did not meet the participation criteria. Eligible participants were then asked a series of demographic questions pertaining to their age, gender, and their clinical practice (e.g., practice duration, practice location, type of clinical practice) and whether they possess a mobile irrespective of who owns it. Those who had a mobile were asked a series of questions pertaining to the mobile(s) such as but not limited to ownership (private, clinical/healthcare workplace, non-clinical/healthcare workplace), apps support, and purposes for which the mobile is used. Those who used a mobile during clinical practice were asked subsequent questions in regards to the mobile that they use during clinical practice such as, but not limited to, questions relating to whether they have used medical apps whilst a patient was present and whether they have used the mobile to take photographs of patients’ wounds. At the end of the survey all participants, irrespective of mobile ownership or use during clinical practice, were asked to indicate their level of agreement (1 = strongly disagree; 5 = strongly agree) with 16 statements on the use of mobiles followed by 14 statements on the use of the internet in clinical practice. Eleven statements on the internet were analogous to the statements on mobiles. Paired samples t-tests were conducted for these analogous statements between mobile phones and the internet.
Results
Forty-three healthcare professionals completed the survey.
Demographics
More females (n = 29) than males (n = 14) participated. Participants had a mean age of 42.3 years (n = 43, SD = 11.1, range = 28-66). Thirty-two healthcare professionals obtained their qualification in Australia. Most participants resided in Victoria (n = 40), whereas the remainder resided in Western Australia (n = 2) and the United States (n = 1). Most participants resided within a capital city (n = 34) whereas the remainder resided in a major urban centre (population: > 100,000) (n = 1), regional city or large town (population: 25,000 – 100,000) (n = 3), smaller town (population: 10,000 – 24,999) (n = 2) and a small community (population: <10,000) (n = 3).
Participants practiced clinically for an average of 16.8 years (n = 43, SD = 9.9, range = 2-40) and on average spent most of their time in clinical practice (65%), followed by research (12%), education (10%), management (10%) and other activities (3%). Seven participants worked within allied health (e.g., physiotherapy, psychology), 20 in medicine (e.g., adult hospital medicine, general practice), 15 in clinical nursing (e.g., hospital theatre, hospital ward), and one as a research nurse.
Recording patient notes for the study
When attending to patients, 27 participants predominantly handwrite notes in the patient’s file, 11 record notes using a desktop computer/laptop/notebook, and the remaining five reported other means (e.g., combination of handwriting notes and using a desktop computer/laptop/notebook). None recorded patient’s notes with a smartphone.
Mobile phone ownership
Most participants (91%) owned a mobile. As can be seen in figure 1, the majority of participants had a privately owned mobile and a large number of them used this mobile for clinical/healthcare work purposes. Furthermore, the majority (84%; 31 out of 37) of participants with a privately owned mobile had one with app support (i.e., a smartphone) (see figure 1). None had a smartphone that was owned by their clinical/healthcare workplace or a non-clinical workplace (see figure 1). The most common reason(s) reported for using their private mobile for clinical/healthcare work purposes was that they have no other mobile (n = 23), followed by that their clinical/healthcare workplace will not provide them with a mobile (n = 10), that it is convenient just to have one mobile instead of having multiple mobiles for different purposes (n = 5), that their privately owned mobile has more functions than their clinical/healthcare workplace mobile (n = 4), other reasons (n = 4) and that their clinical/healthcare workplace reimburses them for using their privately owned mobile (n = 2).
Mobile phone use during clinical practice
Participants were asked to indicate who owns the mobile that they predominantly use during clinical practice and to answer questions pertaining to using this mobile. Most participants used their privately owned mobile during clinical practice (n = 28), whereas the remainder used a mobile owned by their clinical/healthcare workplace (n = 5), and a mobile owned by their non-clinical/healthcare workplace (n = 1). Five participants, who owned a mobile, indicated that they do not use it during clinical practice (see figure 1).
As can be seen in table 1, the most common reason(s) participants used their mobiles was for telephone conversations with healthcare colleagues.
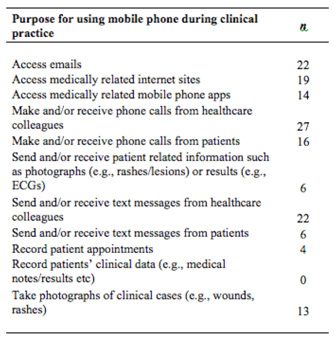
Table 1: Purposes for which healthcare professionals used a mobile phone during clinical practice.
Most participants that used a mobile in clinical practice used a smartphone (24 out of 34; see figure 1). Of these, 83% of participants (i.e., 20 out of 24) were aware that there are medical apps for healthcare professionals. However, when participants were asked whether their clinical/healthcare employer permitted them to use medical apps, four responded with a ‘yes’, whereas the remaining 16 did not know. Those that were permitted to use apps reported that their clinical/healthcare employer did not pay for expenses associated with medical apps. The four participants that used a smartphone within clinical practice, but were unaware of medical apps prior to the survey, indicated that they would consider obtaining them (see figure 1).
Seventy-five per cent of participants (i.e., 15 out of 20) that used smartphones within clinical practice and were aware of medical apps had medical apps on their phone (see figure 1). The most common medical app used was MIMs (n = 7), followed by Uptodate (n = 6), and MedCal (n = 5). Participants most commonly used medical apps a few times per week (n = 6), followed by two or three times per day (n = 4), a few times per month (n = 2), every hour (n = 1), once a day (n = 1), and less than monthly (n = 1). When participants who used medical apps were asked to rate the statement “I find it useful to use medically related mobile phone apps during clinical practice” most answered with ‘agree’ (n = 7) and ‘strongly agree’ (n = 6). The remaining two participants answered with ‘neither agree nor disagree’.
Two thirds of the 15 participants that used medical apps had used a medical app in the presence of their patient. Participants who did not use apps in the presence of their patients did not do so because of the following reason(s): it is not practical to access apps when attending to patients (n = 4), it is unprofessional to use apps in front of a patient (n = 3), there is no time to use apps when attending to patients (n = 2), use of other online resources available on a desktop/laptop/notebook computer (n = 2), and there is no need to use medical apps while attending to patients (n = 2).
The five participants that used a smartphone during clinical practice and were aware of medical apps (see figure 1) but did not have them on their smartphone indicated the following reason(s) for not having them: not knowing how to obtain them (n = 1), finding medical apps too expensive (n = 1), having no need to use medical apps (n = 1), and other (n = 3). The three participants that indicated ‘other’ specified that they preferred to use a computer (n = 2) and that they have not looked for apps or had any recommended to them (n = 1).
The ten participants that used a mobile without app support in clinical practice or were unsure if it had app support were asked if they were aware of medical apps specifically designed for healthcare professionals. Eight of these participants were aware of medical apps (see figure 1). Furthermore, eight of these participants were prepared to obtain a smartphone so that they can access medical apps (see figure 1). The two participants that would not
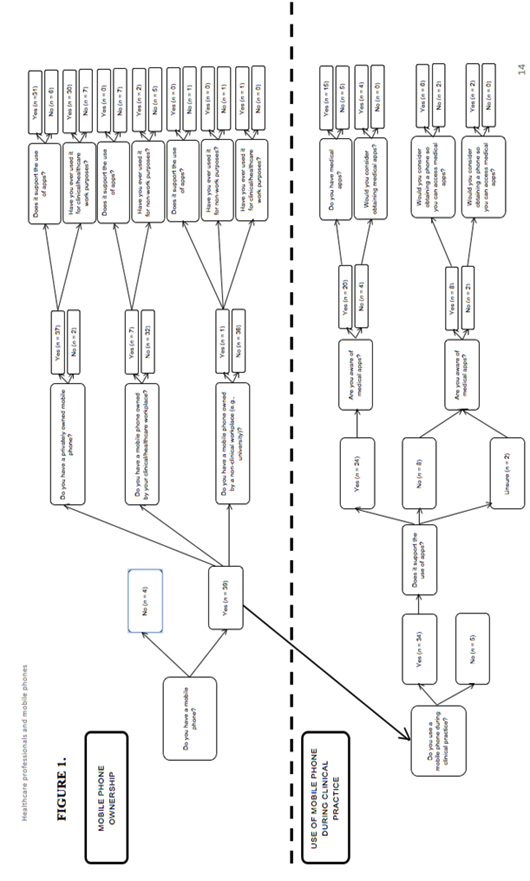
Figure 1. Mobile phone ownership and use during clinical practice.
consider obtaining a smartphone reasoned that they use an iPad instead and that their work decides what phone they will have based on cost.
Attitudes towards the use of mobile phones and the internet in clinical practice
Participants rated eleven analogous statements pertaining to their attitudes towards mobile phone versus internet use in clinical practice (see table 2). Comparison (via paired sample t-tests conducted for these statements) showed that for ten statements attitudes were significantly more favourable towards the internet than mobile phones. However, for eight out of the ten statements showing significant differences between the internet and mobile phones, attitudes towards mobiles were still rated positively. For the remaining two statements mobile phones were perceived negatively. These statements pertained to: 1) confidentiality concerns regarding recording of patient information on mobiles; and 2) healthcare professionals’ perception that patients would assume that their use of mobiles was for non-medical purposes (e.g., texting a friend).
Discussion
Most (91%) healthcare professionals within in our study owned a mobile, and 87% of them used it during clinical practice. Furthermore, 71% of those that use a mobile during clinical practice used a smartphone.
Given the evidence of smartphones assisting clinical practice11,13 and the prevalence of use in our study population, it was surprising to find that only 16% had a mobile phone provided by their clinical/healthcare workplace and of note, none were smartphones. Consequently, most healthcare professionals used their privately owned mobile within clinical practice identifying that this was because their clinical/healthcare workplace did not provide them with one (irrespective of type – i.e., smartphone or non-smartphone).
When healthcare professionals were questioned in regards to use of their mobile within clinical practice it became evident that with the exception of telephone calls, which can be performed on non-smartphones, several other common functions utilised can only be performed on smartphones (e.g., accessing emails, the internet and apps). However, despite a few healthcare professionals having a mobile owned by their clinical/healthcare workplace, none were smartphones. Thus these healthcare professionals could not even utilise functions other healthcare professionals commonly use such as accessing medical apps and the internet.
Although there are many benefits of using smartphones within clinical practice, several concerns regarding these devices have also been highlighted. One such concern pertains to patient confidentiality2,3,17,18. Healthcare professionals’ use of their own mobiles, as commonly reported within our study, appears to be in direct conflict with keeping patient information confidential. For example, patient and private information is likely to be interspersed and thus it is possible that a photograph of a patient’s wound is unintentionally shown to family or friends when using the mobile for private purposes. Of note, despite the prevalence of use of privately owned mobiles within clinical practice in our study, just under half (42%) of all participants indicated that privately owned mobiles should not be used in clinical practice. Furthermore, the attitudinal statement pertaining to confidentially also indicated that participants had significant concerns regarding the use of mobiles to record patient information. An obvious solution would be to supply all healthcare professionals with smartphones so private mobiles are not used within clinical practice. However, this will not automatically resolve the issue regarding patient confidentiality because some healthcare professionals may use their work smartphone for private purposes. It is encouraging to note that two-thirds of healthcare professionals within our study indicated that clinical/healthcare work owned mobiles should not be used for private purposes. The idea of supplying healthcare professionals with smartphones does not entirely resolve concerns regarding patient confidentiality; it would be a step in the right direction as healthcare professionals can be encouraged to minimise private information on work owned smartphones. On the other hand, if healthcare professionals were expected to use privately owned mobiles within clinical practice then one could not impose regulations on how these devices are to be used for non-work purposes. Interestingly, 80% of our study participants that used a smartphone in clinical practice and were aware of medical apps were unsure if their workplace permitted the use of apps. This clearly is an area that needs further consideration.
Another concern regarding the use of mobiles within clinical practice pertains to cross-infection3,12,15. One quarter of healthcare professionals within our study expressed concerns regarding cross-infection when using smartphones to access apps whilst attending to patients. Perhaps healthcare
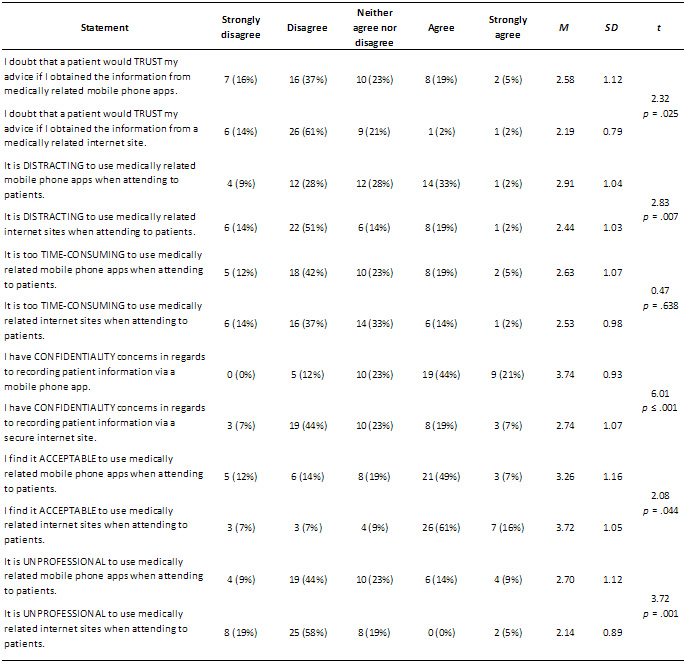
Table 2. Healthcare professionals’ attitudes towards the use of mobile phones and the internet in clinical practice. Descriptive statistics of participants’ levels of agreement (1 = strongly disagree; 5 = strongly agree) with 16 statements on the use of mobiles and 14 statements on the use of the internet in clinical practice are shown. Paired samples t-tests were conducted for the 11 analogous statements between mobile phones and the internet. Please note: participants rated all statements pertaining to mobile phones before they rated statements pertaining to the internet. Within each set of ratings, statements were presented in a random order (i.e., not in the order presented here).
Some statements were adapted from Koehler et al. (2013).19
professionals’ cross-infection concerns relate to the fact that as portable devices mobiles may be used between patient encounters with a subsequent cross-infection risk should healthcare professions not wash their hands.
Overall we found that healthcare professionals generally had more favourable attitudes towards internet than mobile use within clinical practice. Despite mobiles being more accessible than the internet via a desktop / laptop given that mobiles are portable, healthcare professionals found medical apps to be more distracting to use than medical internet sites. Furthermore, healthcare professionals had more confidentiality concerns associated with recording patient information via an app than an internet site and felt that patients would trust their advice less if they obtained information from an app than the internet.
Healthcare professionals found it more acceptable and less unprofessional to use the internet than apps when attending to patients. These perceptions even extend to what they perceive others think they are doing when using these devices. Healthcare professionals were more likely to be concerned that a patient would think that they are using a device for non-work related purposes if they were seen using their mobile than when seen using the internet.
Healthcare professionals’ concerns in regards to being perceived to use a mobile for non-work purposes depended on whom they were seen by when using the device. Healthcare professionals were more likely to be concerned that patients seeing them use a mobile would think they are using it for non-work purposes as opposed to being seen by a fellow healthcare professional. Given the ease of being able to perform non-work related tasks (e.g., personal texts) on mobiles it is not surprising that some healthcare professionals have the concern that others think they are using the device for non-work purposes. Furthermore, healthcare professionals may think that patients are not aware that smartphones can be used for medical purposes and thus patients may erroneously perceive the device is being used for non-work purposes. Interestingly healthcare professionals are more likely to think that their colleagues perceive them as using mobiles for non-work purposes than they are to think this of their colleagues.
Several of the attitudinal differences in regards to using a mobile compared to the internet in clinical practice could be attributed to the internet preceding mobiles. Therefore individuals may be less familiar with the role mobiles can play in clinical practice and thus an erroneous perception may have formed that they function more as social media tools than tools facilitating medical care. In contrast the internet is commonly used in educational and work settings and thus may be perceived as facilitating medical care more so than mobiles.
In regards to using technology compared to traditional means of locating information such as in textbooks, healthcare professionals generally preferred to use technology and this was more so for the internet than apps. This can possibly be explained by it being easier and quicker to conduct an electronic search than flicking through numerous textbooks or other paper based materials. Furthermore, 67% believed that medically related internet sites will replace non-electronic resources within 10 years whereas only 47% believed the same in regards to medical apps.
When healthcare professionals were asked in regards to obtaining information on the internet, 79% would use an internet search engine (e.g., Google) to search for an unfamiliar clinical condition. Furthermore, 70% would be more likely to use an internet search engine, than an online peer reviewed journal, to obtain additional clinical information while attending to a patient. This result is quite concerning given that the content of information retrieved from online searches is not always reliable. However, it is reassuring to note that only 17% used Wikipedia more frequently than online journals to obtain clinical information. These results suggest that most healthcare professionals do make appropriate judgements when viewing online material. In contrast, despite no formal review process existing for medical apps, only 16% of healthcare professionals perceive the content of medical apps to be unreliable. Overall, these findings suggest that healthcare professionals should be cautious in regards to the material they access and that a formal review process (i.e., similar to that for journal articles) should be implemented for medical apps. Three quarters of healthcare professionals who used smartphones within clinical practice and were aware of medical apps used medical apps within clinical practice. This number is likely to rise with an increasing number of healthcare professionals obtaining smartphones and becoming aware of medical apps. Thus if medical apps are to have a future within healthcare then having some quality assurance in regards to an apps’ content, via a formal review process, is paramount to ensure patient safety.
Limitations
Despite our best efforts to recruit as many healthcare professionals within Australia as possible our sample size is relatively small. Our small sample size could be attributed to healthcare professionals generally being over surveyed and healthcare professionals having limited time within their busy profession to complete surveys.
Given that healthcare professionals are time poor we chose to collect data via an on-line survey because it is quicker to complete a survey by this means than to complete and return a paper based survey via physical mail. However, using an on-line data collection method (i.e., excluding healthcare professionals who do not use the internet) poses a selection bias for our study in that healthcare professionals within our study are likely to have positive attitudes towards using the internet given that they completed the survey on-line.
Our study is also limited in that we did not obtain information in regards to healthcare professionals’ use of and attitudes towards tablets in clinical practice. With the exception of one participant who stated in a written response to a question that they used an iPad we are unaware as to whether healthcare professionals within our study owned tablets. Such knowledge is important because those who do not have a smartphone may use a tablet instead and thus would have access to similar functions that can be accessed on smartphones such as medical apps. Thus to obtain a more comprehensive understanding of the use of new technology in clinical practice future studies should also include tablet use.
Conclusions
Our study shows that mobiles, including smartphones, are commonly used within clinical practice and that at present most healthcare professionals use their privately owned device. Despite this, most healthcare professionals had reservations pertaining to mobile use within clinical practice, including the use of privately owned mobiles and the potential for confidentiality breaches and cross-infection. When comparing attitudes towards the internet and mobile phones, in general attitudes towards both were favourable but more so for the internet. This study demonstrates a level of discordance between participants’ behaviours and their attitudes towards mobile phone use within clinical practice. In addition, many participants were uncertain as to whether the use of medical apps was permitted at their clinical/healthcare workplace. Clearly smartphones already have a significant function in clinical practice. However, their role and appropriateness in clinical practice requires further research. In conclusion, these findings suggest that smartphones may become a key resource within clinical practicein the future.
Acknowledgements
The study reported here is part of a larger study which examined individuals’ attitudes towards healthcare professionals using mobile phones within clinical practice. Thus the survey questions within this study are very similar to that reported within our previous study19. Dr Nicole Koehler was employed within the Faculty of Medicine, Nursing and Health Sciences at Monash University at the time this study was conducted.
References
1. Australian Bureau of Statistics, 2012, Household Use of Information Technology, Australia, 2010-11, cat. no. 8146.0, viewed 5 April 2012, http://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/4E4D83E02F39FC32CA25796600152BF4?opendocument
2. Boulos, M. N. K., Wheeler, S., Tavares, C., & Jones, R. (2011). How smartphones are changing the face of mobile and participatory healthcare : An overview, with example from eCAALYX. Biomedical Engineering Online, 10, 24. ![]()
3. Phillippi, J. C., & Wyatt, T. H. (2011). Smartphones in nursing education. Computers, Informatics, Nursing, 29, 449-454. ![]()
4. Havelka, S. (2011). Mobile resources for nursing students and nursing faculty. Journal of Electronic Resources in Medical Libraries, 8, 194-199. ![]()
5. Dasari, K. B., White, S. M., & Pateman, J. (2011). Survey of iPhone usage among anaesthetists in England. Anaesthesia, 66, 620-631. ![]()
6. Franko, O. I., & Tirrell, T. F. (2011). Smartphone app use among medical providers in ACGME training programs. Journal of Medical Systems [Online]. Available: http://springerlink.com/content/p6t82ph541835u75/
7. Franko, O. I. (2011). Smartphone apps for orthopaedic surgeons. Clin Orthop Relat Res, 469, 2042–2048.
8. Baumgart, D. C. (2011). Smartphones in clinical practice, medical education, and research. Archives of Internal Medicine, 171, 1294-1296. ![]()
9. Fried, J. J. (2012). Images at your fingertips. Community Oncology, 9, 141-142. ![]()
10. Savel, R. H., & Munro, C. L. (2011). Scalpel, stethoscope, iPad: The future is now in the intensive care unit. American Journal of Critical Care, 20, 275-277. ![]()
11. Flannigan, C., & McAloon, J. (2011). Students prescribing emergency drug infusions utilising smartphones outperform consultants using BNFCs. Resuscitation, 82, 1424-1427. ![]()
12. Josephson, C. B., & Salman, R. A-S. (2010). Smartphone: Can an iPhone app help stroke physicians? The Lancet, 9, 765.
13. Low, D., Clark, N., Soar, J., Padkin, A., Stoneham, A., Perkins, G. D., & Nolan, J. (2011). A randomised control trial to determine if use of the iResus application on a smart phone improves the performance of an advanced life support provider in a simulated medical emergency. Anaesthesia, 66, 255-262. ![]()
14. Zanner, R., Wilhelm, D., Feussner, H., Schneider, G. (2007). Evaluation of M-AID, a first aid application for mobile phones, Resuscitation, 74, 487-494. ![]()
15. Osborne, J. D. D., Phull, J. S., & Matone, L. I. (2012). Might wipe clean covers for mobile phones reduce risk of spread of pathogens? British Medical Journal, 344, e871. ![]()
16. van Lieshout, E. J., van der Veer, S. N., Hensbroek, R., Korevaar, J. C., Vroom, M. B., & Schultz, M. J. (2007). Interference by new-generation mobile phones on critical care medical equipment. Critical Care, 11:R98. ![]()
17. Nolan, T. (2011). A smarter way to practise. British Medical Journal, 342, d1124. ![]()
18. Burns, K., & Belton, S. (2012). “Click first, care second” photography. Medical Journal of Australia, 197, 265. ![]()
19. Koehler, N., Vujovic, O., & McMenamin, C. (2013). Are individuals more accepting of the internet than mobile phone apps being used in clinical practice? Journal of Mobile Technology in Medicine, 2: 14


0 Comments
Trackbacks/Pingbacks