Simple, Low-Cost Smartphone Adapter for Rapid, High Quality Ocular Anterior Segment Imaging: A Photo Diary
David Myung, MD PhD1, Alexandre Jais, MS1, Lingmin He, MD MS1, Robert T. Chang, MD1
1Byers Eye Institute at Stanford, Stanford University School of Medicine, Stanford, California
Corresponding Author: viroptic@gmail.com
Journal MTM 3:1:2–8, 2014
Background: Smartphones with high quality photographic and video capabilities are now ubiquitous. However their utility for documenting ocular pathology has been limited by the optics, magnification, and lighting control required to capture key anatomic details of the eye. While various adapters have been designed to attach a smartphone to a slitlamp to obtain clinically useful photos, we sought a way for practitioners to achieve similar photos using only their existing smartphones with minimal additional hardware.
Methods: We report the design of a simple, point-of-care optical adapter for imaging the anterior segment that combines a low-cost macrolens, LED external light source, and a universal attachment system for use with all smartphones. The adapter is easily attached and detached from a phone in seconds and is small enough to fit in a pocket when not in use.
Results: A series of anterior segment photographs were obtained with the adapter that satisfactorily portrays a wide range of pathology of the eyelids, conjunctiva, cornea, iris, and lens without the need for a slitlamp. The external LED adjacent to the macrolens was key in creating a single light reflex that eliminated reflections on the cornea caused by ambient light.
Conclusions: A simple, low-cost smartphone adapter can provide useful clinical information regarding the appearance of the lids and lashes, the clarity of the cornea, the state of the conjunctiva, the shape of the pupil and health of the iris, and the presence or absence of a hyphema or hypopyon. This may be useful for urgent triage and teleophthalmology in various settings.
Introduction
The widespread adoption of the modern smartphone now allows everyone, including physicians, to easily capture photographs and videos during a patient encounter. This trend is poised to explode as seamless mobile data encryption and uploading to cloud storage becomes widespread. A number of adapters exist that enable practitioners to capture ophthalmic anterior segment photos by attaching an iPhone or equivalent to a slitlamp microscope or direct ophthalmoscope via simple adapters that mount the smartphone to one of the oculars.1–4 Two commercial examples of these are the iExaminer (Welch Allyn, Skaneateles Falls, NY) and the EyePhotoDoc system developed at the Terry Eye Institute (eyephotodoc.com). Our group sought a way to simplify ocular image capture with a smartphone that did not require a slit lamp or specialized training.
Our group designed a “minimalist” optical system for imaging the anterior segment from the ground up that combines the following three elements (1) a low-cost macrolens, (2) a properly positioned LED light, and (3) a mounting system universal to all smartphones. Here, we report the development of our first generation, compact, user-friendly, attachment and clinical photos obtained with it. The key feature is that it is a lightweight low-cost adapter that reversibly couples with the iPhone 4 and higher. With it, we were able to quickly photodocument a variety of anterior segment pathologies without the need for a slitlamp.
Methods
Optical element
Several smartphone macrolenses for general use are commercially available today. Many of them, such as the Olloclip (which was one of the first such macrolens attachments available), are custom designed for a particular iPhone model. Our initial work was done with an Olloclip, but the model we purchased soon became unusable once the iPhone 5 was released, which not only had a better camera but also was substantially thinner and thus was no longer compatible with the lens. We subsequently found a number of “universal” macrolens fittings for smartphones that not only were agnostic to phone make and model, but also were significantly cheaper ($10-$20 versus the $70 for the Olloclip).
Illumination
All the macrolenses on the market provided adequate optical zoom at an acceptable working distance (about 2.5 cm) from a patient’s face. The problem with using these to photograph the eye was the lighting. Ambient lighting led to background reflections on the surface of the cornea, obscuring important details. When the iPhone native flash was used in “torch” mode (with the macrolens covering the camera lens but not the adjacent flash), patients found the light to be too intense, and, at the same time, photos were over-exposed. This was the case even when the intensity was reduced with filters or by using the FilmicPro application (available on the iTunes app store), which is currently the only one on the market that we are aware of provides control over flash intensity.
After multiple attempts, we learned that reflections caused by ambient lighting can be best minimized by the creation of a single corneal light reflex. On a slitlamp system, this is provided in two ways: first, by the slitbeam itself, and second, through a reflected light source that creates a flash emanating inferiorly at the time of photocapture. In our experience, the iPhone stock camera is able to take excellent and arguably better resolution photos without a flash than it does with a flash. Thus, we decided that an external LED would simultaneously provide (a) a level of illumination that would be comfortable for the patient, (b) the right amount of exposure, and (3) a single light reflex that eliminates reflections on the cornea.
After much brainstorming, prototyping, and iterations, two designs were employed. Both designs utilize a macrolens with universal clip (CamKix, Inc.) capable of positioning the macrolens on nearly any smartphone on market today, including both Apple and Samsung devices. The benefit of the universal clip was that it could also be used in the presence of a case, which typically adds anywhere from 1-3 mm of additional thickness to a phone, and is relatively inexpensive (about $12 through various online distributors, including Amazon.com).
An LED light source was then fixed to the lens clip with or without plastic (ABS) spacers using commercially available adhesives. In version 1, the light was redirected with a mirror placed just below the macro lens (Figure 1). In version 2, the light was redirected with a plastic endcap, thus providing direct light rather than reflected light (Figure 1c).
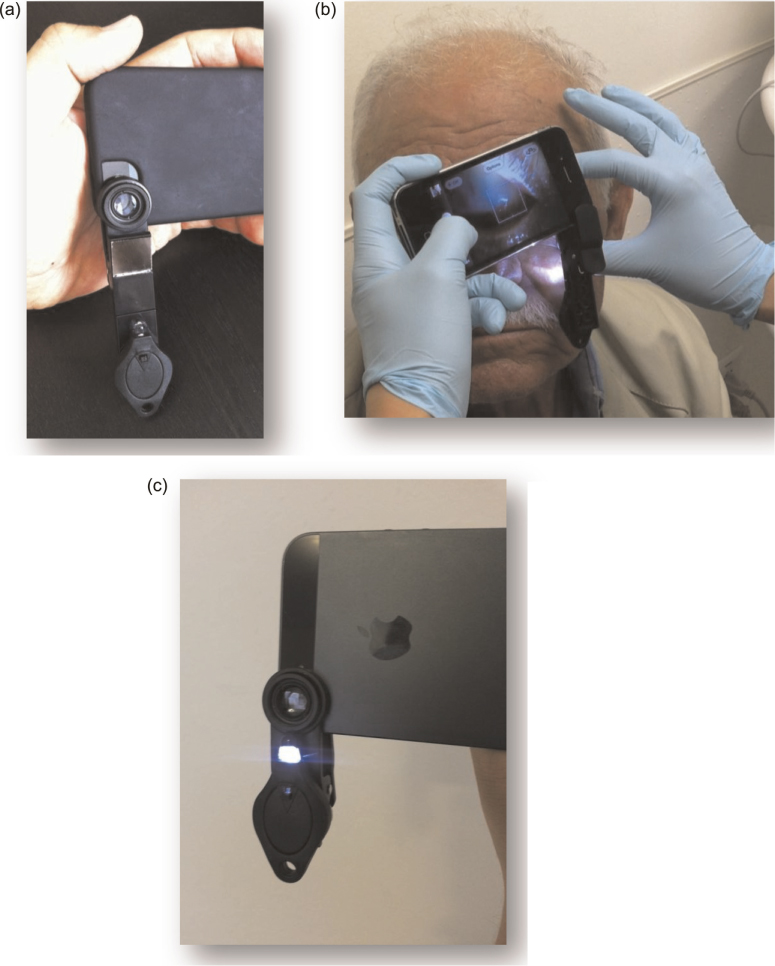
Figure 1: (a) Prototype lens adapter with reflected LED illumination. (b) Photo showing the lens adapter in Figure 1 being used with an iPhone 4S to capture an image of the anterior segment of a patient’s eye. (c) Prototype lens adapter with direct LED illumination
The focal length of the macro lens is approximately 2.5 cm, so the device is held adjacent to the patient’s eye as shown in Figure 1b. We found that the optimum way to take photos with the adapter is as follows. The phone is held in part with two hands; one hand is used to hold the phone on one end between the third finger and thumb, while the fourth, and fifth digits are used to stabilize the phone with gentle contact with the patient’s head. The other hand is used to further stabilize the phone. The index finger of the handclosest to button on the camera is used to take the photo.
Because of the required proximity between the phone and the patient’s face, care must be taken in all cases to not allow contact between the phone and adapter and the patient’s skin, especially in those who have a periorbital rash or injury (such as a laceration). In the event contact is made, the adapter and phone can be wiped clean with an alcohol swab; the adapter itself can be submerged in soap and water or another cleaning solution.
For protection of privacy, photographs taken with these adapters are being transmitted either through (1) the EPIC Haiku mobile application, that enables direct upload of photos to a patient’s medical record, (2) secure, encrypted institutional email, or (3) a HIPAA-compliant messaging application called Medigram (Los Altos, CA), which has been approved and is being deployed by the Stanford Hospital IT department for the capture and transmission of textpages and photos. All phones that are used to capture images are encrypted using the university or hospital Mobile Device Management (MDM) application. All image acquisition and transmittal was handled with strict attention to the confidentiality of personal data in accordance with the Data Protection Act of 1998 and Access to Health Records of 1990.
Results
Macro lenses for smartphones have been on the market for sometime, such as the Olloclip, Easy-Macro Lens, and other examples. Proper illumination was the main challenge in trying to obtain maximum level of detail of the ocular surface without unwanted background reflections that obscure detail of the actual eye. Figure 2a-b below exemplifies this difference:
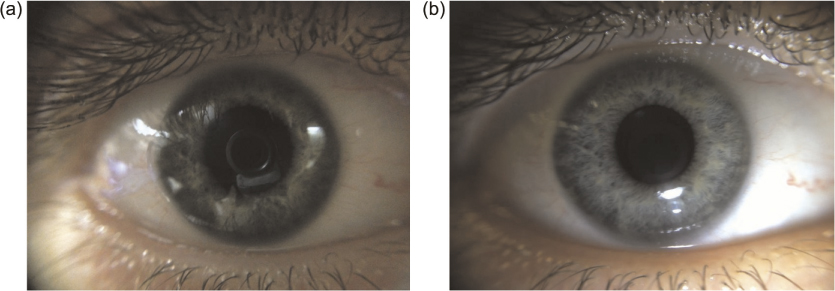
Figure 2: (a) Photograph of ocular surface with macro lens alone, without LED illumination. (b) Photograph of ocular surface of same patient using reflected LED illumination from adapter shown in Figure 1
Figure 3a-b juxtaposes photos of a patient’s eye using only the stock camera app and lens (Figure 3a) and the same stock camera app used in conjunction with the macrolens and LED (Figure 3b) shown in Figure 1a. Both photographs were taken without the use of the digital zoom function available on the iPhone. We found that digital zoom could be used in the absence of the macrolens and light source, but that this caused a reduction in image quality compared to the optical zoom provided by the macrolens, and the lack of proper illumination using digital zoom alone led to unwanted corneal reflections. The phone’s native flash, which is adjacent to the camera lens, was also used in “torch” mode to take photos in combination with the digital zoom function; we found that these images were of poorer quality compared to the combination of macrolens and LED setup described here.
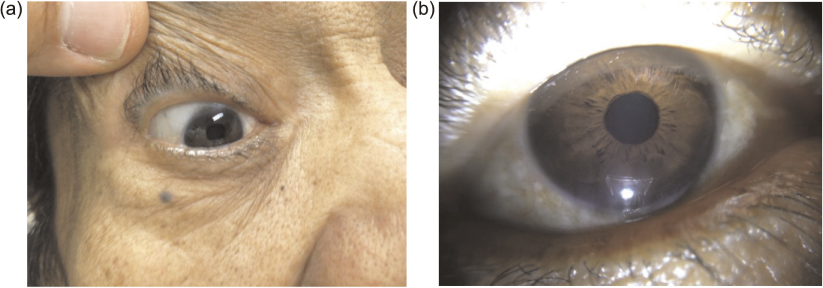
Figure 3: (a) Photograph of patient’s eye using iPhone camera alone. (b) Photograph of same patient’s eye using iPhone camera and adapter shown in Figure 1a
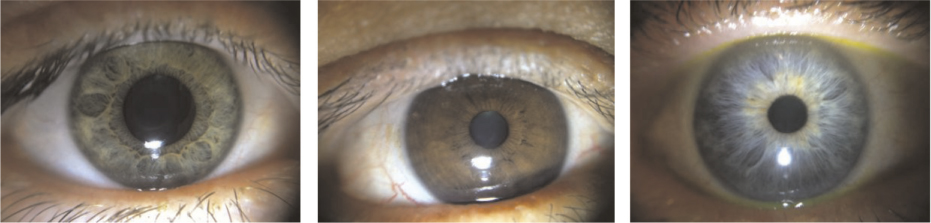
Figure 4: Green (left), brown (middle), and blue (right) irides of patients with normal, healthy anterior segments
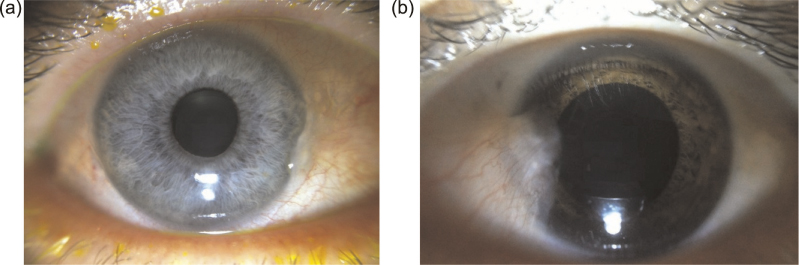
Figure 5: (a) A nasal pingueculum. (b) A nasal pterygium
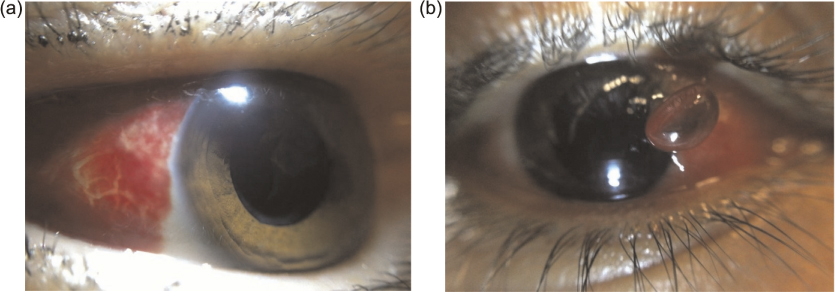
Figure 6: (a) Subconjunctival hemorrhage. (b) Pyogenic granuloma
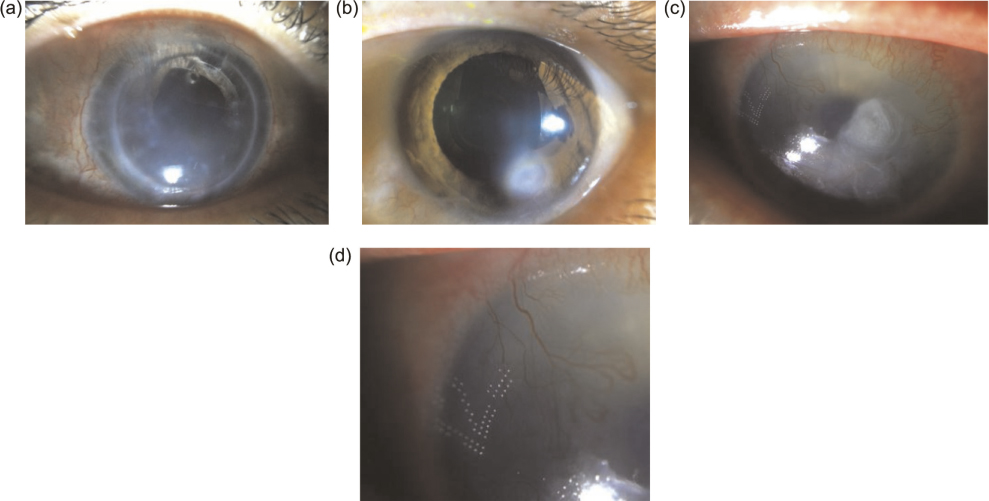
Figure 7: (a) Corneal graft failure. (b) Corneal ulcer, without fluorescein. (c) Perforated cornea with corneal glue and bandage contact lens applied
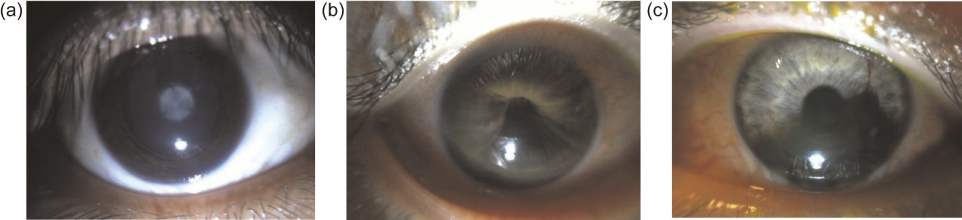
Figure 8: (a) Fetal cataract showing both upright and inverted Y sutures. (b) Iris bombe. (c) Hyphema

Figure 9: (a) Herpetic lid margin disease. (b) Staph marginal keratitis with fluorescein staining
The following is a photodiary of images taken with adapters in Figures 1a and 1b. We found that the image quality was identical between the two types of illumination. All photographs of patients’s eyes were taken with their permission.
We found that to image fluorescein staining, no separate blue light was needed, and that white LED illumination was sufficient. We are developing a version of this adapter that incorporates the option of blue LED illumination, which may provide additional finer details of more punctate or subtle fluorescein staining patterns.
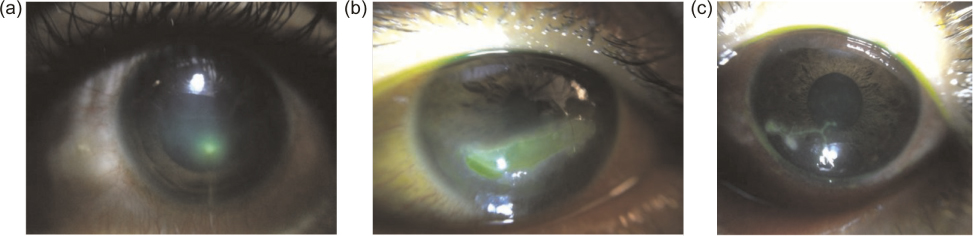
Figure 10: (a) Fluorescein staining of a corneal ulcer. (b) Fluorescein staining of a corneal abrasion. (c) Fluorescein staining of herpetic dendrite
Discussion
Our photodiary demonstrates the proof of concept that high quality anterior segment images can be easily and reproducibly captured by the lens adapter described, coupled with an iPhone 4 or higher and the stock camera application. Our design is believed to be an improvement for ease-of use and cost-effectiveness as the adapter bypasses the need for a slitlamp for capturing high magnification and well-illuminated images of the ocular surface, with a total cost of goods of less than $15 for the mechanical prototypes described herein. Our primary criteria for image quality was iris detail; when iris detail was in focus, the majority of the ocular surface would come into the appropriate focus. We have an ongoing IRB-approved study at our institution directed toward evaluating the quality of the photos taken with this adapter.
Important limitations of the current adapter is the inability to create a slit of light that would be useful in estimating depth of corneal pathology, and for capturing cell and flare. However, we feel that images captured with the current adapter provides sufficient information with regard to the (1) clarity of the cornea, (2) quality of the epithelium, (3) fluorescein uptake, (4) the state of the conjunctiva (whether it is injected, chemotic, or hemorrhagic), (5) the shape of the pupil, (6) the health of the iris, (7) the presence or absence of a hyphema or hypopyon in the anterior chamber, and (8) the appearance of the lids and lashes.
Another potential drawback is the close working distance of the macrolenses (about 2.5 cm). Currently we recommend using an alcohol swab to wipe down the adapter and case of the phone after use (or use soap and water on the adapter alone). However, we are also exploring the possibility of using a lens with a slightly longer focal distance.
Conclusions
The combination of secure message transmission, smartphones with cloud access and high quality camera technology, and a user-friendly, low cost adapter to easily couple lenses to a smartphone are now making teleophthalmology increasingly accessible. We have concurrently been developing a low-cost posterior segment imaging adapter for smartphones as well. Our ultimate goal is for this system to be usable by healthcare staff with minimal specialized training to remotely capture and share high quality anterior segment images in order to enhance healthcare provider communication. An example would be enabling a triage nurse to text a secure, reliable image to an ophthalmologist on-call. In future work, we plan to deploy subsequent generations of the adapter to non-ophthalmologists to evaluate their potential use in developing nations, inpatient consults, and areas where access to an ophthalmologist is limited.
Disclosure
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf and declare: a patent pending on the submitted work but no support from any organization for the submitted work and no financial relationships with any organizations that might have an interest in the submitted work.
References
1. Hester C. Available at: http://eyewiki.aao.org/Smart_Phoneography_-_How_to_take_slit_lamp_photographs_with_an_iPhone.
2. Teichman JC, Sher JH, Ahmed IIK. From iPhone to eyePhone: A technique for photodocumentation. Canadian Journal of Ophthalmology/Journal Canadien d’Ophtalmologie 2011;46(3):284–6.![]()
3. Lord RK, Shah VA, San Filippo AN, Krishna R. Novel uses of smartphones in ophthalmology. Ophthalmology 2010;117(6):1274. e3.![]()
4. Chakrabarti D. Application of mobile technology in ophthalmology to meet the demands of low-resource settings. Journal of Mobile Technology in Medicine 2012;1(4S):1–3.![]()
5. Haddock LJ, Kim DY, Mukai S. Simple, Inexpensive Technique for High-Quality Smartphone Fundus Photography in Human and Animal Eyes. Journal of Ophthalmology 2013;2013.
6. Bastawrous A. Smartphone fundoscopy. Ophthalmology 2012;119(2):432–3. e2.![]()
7. Chhablani J, Kaja S, Shah VA. Smartphones in ophthalmology. Indian J Ophthalmol 2012;60(2):127.

