Contextual Barriers to Mobile Health Technology in African Countries: A Perspective Piece
Yvonne O’ Connor, PhD1, John O’ Donoghue, PhD2
1Health Information Systems Research Centre, University College Cork, Cork, Ireland; 2Global eHealth Unit, Imperial College London, UK
Corresponding Author: y.oconnor@ucc.ie
Journal MTM 4:1:31–34, 2015
On a global scale, healthcare practitioners are now beginning to move from traditional desktop-based computer technologies towards mobile computing environments1. Consequently, such environments have received immense attention from both academia and industry, in order to explore these promising opportunities, apparent limitations, and implications for both theory and practice2. The application of mobile IT within a medical context, referred to as mobile health or mHealth, has revolutionised the delivery of healthcare services as mobile technologies offer the potential of retrieving, modifying and entering patient-related data/information at the point-of-care. As a component of the larger health informatics domain mHealth may be referred as all portable computing devices (e.g. mobile phones, mobile clinical assistants and medical sensors) used in a healthcare context to support the delivery of healthcare services.
The usefulness of implementing IT in healthcare is reflected in current eHealth initiatives in resource-poor settings (e.g. Baobab Health in Malawi, M-Pedigree in Ghana, Nigeria and Kenya; Cell-Life in South Africa). In recent years attempts have being made to digitise WHO/UNICEF paper-based clinical guidelines when delivering paediatric healthcare services, namely: Integrated Management of Childhood Illness (IMCI) and Community Case Management (CCM). Both IMCI and CCM are stepwise and structured approaches, employed by Community Health Workers (CHW), towards reducing death, illness and disability while promoting improved growth and development among children under five years of age3,4. Digitising the IMCI and CCM guidelines offer profound opportunities to CHW (also referred to as Health Surveillance Assistants in Malawi, Africa) in terms of improving adherence to clinical guidelines, offering instant access to patient data independent of location and time and facilitating drug ordering via Short Message Service (SMS)5.
However, introducing mobile technology in a medical context within resource-poor communities is not without its challenges6. One obstacle faced by mHealth users is lack of user acceptance of the technology. Common factors which influence the decision making process of accepting mobile technology in medicine may include perceived usefulness, perceived ease-of-use of the technological tool7, performance expectancy, effort expectancy, social influence, facilitating conditions8. Arguably, the most imperative barrier faced by mHealth users in Africa is that of a contextual nature. The underlying premise behind this argument is that many mHealth solutions for use in developing countries are often developed in western societies. Such solutions have been criticised for failing to recognise the unique contextual factors associated with developing regions9. Contextual factors reflect external or driving elements that comprise the environment or conditions for decision making tasks10 and as a result, such factors can vary across populations and industries. Cultural, economic, political and cognitive dimensions are contextual factors which could influence how end users interact with mobile technology in medicine (referenced 1–4, Figure 1).
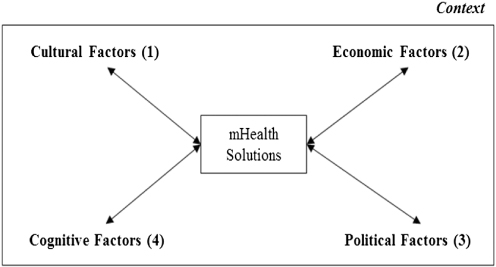
Figure 1: Contextual factors which should be incorporated into mHealth solutions
Cultural factors (1, Figure 1) denote a set of beliefs and norms that are both consciously and subconsciously held by any individual in the given society11. In the context of this paper, this refers to the principles/customs held by CHW in rural regions of Africa. Culture diversity between developing and developed countries can be observed based on “Individualism versus Collectivism”, “Power distance”, and “Masculinity versus Femininity”12. That is, developed countries such as Europe and U.S.A. are driven by individualist approaches whereas developing countries are concerned with collectivist strategies. Power distance reflects the way society distributes, shares, and enforces the power among its members13. Power holders in high power distance cultures such as Africa are much more comfortable with a larger status differential than low power distance cultures. Additionally, research in African countries shows preferential treatment towards males over females. It is worth noting, however, that cultural values cannot be easily adjusted to conform to any changes introduced by mHealth. This conformity, therefore, may have an impact on individual users’ intentions to adopt mHealth technologies in Africa. The authors suggest that ethnographic studies should be performed to capture local cultural dimensions similar to the work of Kitson (2011)14. In her work Kitson identified a number of cultural factors impacting the implementation of the Care2x hospital information system in Tanzania.
Economic factors (2, Figure 1) refer to the direct and indirect financial opportunities attributable to CHW in rural areas of developing regions. Without the necessary economic support for sufficient tools and resources, technology transfer from developed regions to Africa becomes very complicated, given the existing technological infrastructures at many African locations15. To help ensure that mHealth solutions are a viable option for African countries a cost analysis should be performed as advocated by Schweitzer and Synowiec (2012)16. Increased mobile coverage in rural areas, including faster network connectivity, is essential to realising the potential and scope of mHealth in developing countries. However, western societies should develop solutions that operate on commonly used mobile devices in developing regions. Many mHealth initiatives in Africa utilise the SMS functionality of mobile communication systems as a core connectivity method. The underlying rationale for using this low-cost functionality is that high-performance devices are not required to transmit data. For example, the effects of mobile phone SMS on antiretroviral treatment adherence in Kenya was examined17,18. These studies provide empirical evidence that mobile health initiatives can improve HIV treatment outcomes.
Political factors (3, Figure 1) refer to the governmental agenda of central administrations within developing regions. The planning and budgeting process in resource-poor areas are often constrained by expenditures in previous years. As a result, developing regions often face difficulty to mobilise funds for full-scale mHealth implementation as there may be no reliable or guaranteed governmental financial support for sustaining mHealth initiatives. If mobile technologies are to be successfully introduced across healthcare within developing regions, it is an essential that government agencies provide the necessary support, such as local Ministries of Health and local software industries to manage and maintain the software artefact. EHealth Nigeria is an example whereby an organisation collaborates closely with appropriate political powers to ensure the sustainability of Health Management Information Systems.
Cognitive factors (4, Figure 1) refer to users’ personal self-beliefs and opinions ability to interact with mobile technologies in a medical domain. That is, the degree to which a CHW perceives his or her ability to use mHealth technologies in the accomplishment of a task19. Cognitive dimensions do play an integral role in the use of mHealth technologies in developing countries as it is reported that such regions face education limitations (computer illiteracy) and a lack of English language skills. Research conducted in the health domain of Mozambique revealed that a limited amount of participants were computer literate, with only a minority of health workers at health facilities having the cognitive ability to interpret health data20. MHealth initiatives promoted by developed countries are often developed using the English language. This can hinder the use of mobile technology in medicine due to the lack of language translation abilities implemented within the software solution. It is therefore imperative that developers facilitate multi-language support to enhance the usability of mHealth technologies. Furthermore, training workshops should be provided to end users of mHealth solutions to enhance proficiency with the technology21. The importance of providing training workshops is reflected in the work performed by Baobab health in Malawi. They offer initial and refresher training courses to end users of their eHealth systems arguing that training is essential.
Conclusion
The status quo of the healthcare sector in Africa is plagued with uncertainty surrounding lack of resources (financial, technical and human), inadequate training to support health care providers, lack of technical infrastructure, limited participation in the development of medical/clinical standards, and lack of understanding of standards at national level)9. As a result, extant research on IT in the less-developed world has been severely limited. To add to this complexity IT solutions designed in developed countries have often failed to transfer effectively to African regions. To ensure that mHealth is a viable option for the health services sector in African countries many eHealth initiatives are attempting to address contextual factors as part of their development. This perspective piece argues that it is imperative for developers to encompass local cultural, economic, political and cognitive factors to ensure intentions, use and diffusion of mHealth initiatives.
Acknowledgements
“The Supporting LIFE project (305292) is funded by the Seventh Framework Programme for Research and Technological Development of the European Commission www.supportinglife.eu”
References
1. Wu J-H, Shu-Ching W, Li-Min L. Mobile computing acceptance factors in the healthcare industry: A structural equation model. International Journal of Medical Informatics 2007;76:66–77. ![]()
2. Kjeldskov J, Skov M. Exploring context-awareness for ubiquitous computing in the healthcare domain. Personal and Ubiquitous Computing 2007;11:549–62. ![]()
3. Handbook: IMCI management of childhood illness. 2005 edition. Geneva and New York, WHO and UNICEF, 2005. Available: http://whqlibdoc.who.int/publications/2005/9241546441.pdf
4. CORE Group, Save the Children, BASICS and MCHIP, 2nd Edition 2012. Community Case Management Essentials: Treating Common Childhood Illnesses in the Community. A Guide for Program Managers. Washington, D.C. Available: http://www.coregroup.org/storage/documents/CCM/CCMEssentialsGuide/ccmbook2012-online.pdf
5. Mitchell M, Getchell M, Nkaka M, Msellemu D, Van Esch J, Hedt-Gauthier B. Perceived improvement in integrated management of childhood illness implementation through use of mobile Technology: qualitative evidence from a pilot study in Tanzania. Journal of Health Communication 2012;17:118–27. ![]()
6. Mechael PN. The case for mHealth in developing countries. Innovations 2009;4:103–18. ![]()
7. Davis FD Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly 1989;13:319–40. ![]()
8. Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Quarterly 2003;27:425–78.
9. Avgerou C. Information systems in developing countries: a critical research review. J Inf technol 2008;23:133–46. ![]()
10. Fjerrnestad, J, Hiltz, SR. Experimental Studies Of Group Decision Support Systems: An Assessment Of Variables Studied And Methodology. In: Proceedings of the Thirtieth Hawaii International Conference on System Sciences, IEEE 1997: 45–65
11. Adler NJ. International Dimensions of Organizational Behavior. Cincinnati: South-Western College Publishing 2002.
12. Hofstede G. Culture’s Consequences: International Differences in Work-Related Values. Beverly Hills CA: Sage 1980.
13. Al-Abdul-Gader, AH. Managing Computer Based Information Systems In Developing Countries: A cultural perspective, IGI Global 1999.
14. Kitson N. A Convergence of Cultures and Strategies to Improve Electronic Health Record Implementation within a Tanzanian Clinical Environment. University of Alberta 2011.
15. Jimenez-Castellanos, A, de la Calle, G, Alonso-Calvo, R, Hussein, R, Maojo, V. Accessing advanced computational resources in Africa through cloud computing. 25th International Symposium on Computer-Based Medical Systems (CBMS), 2012: 1–4.
16. Schweitzer J, Synowiec C. The economics of eHealth and mHealth. Journal of Health Communication 2012;17:73–81. ![]()
17. Lester, RT, Mills, EJ, Kariri, A, Ritvo, P, Chung, M, Jack, W, et al. “The HAART cell phone adherence trial (WelTel Kenya1): a randomized controlled trial protocol.” Trials 2009 Sep 22;10:87. ![]()
18. Douglas G, Gadabu O, Joukes S, Mumba S, McKay M, Ben-Smith A, Jahn A, Schouten E, Lewis Z, van Oosterhout J. Using touchscreen electronic medical record systems to support and monitor national scale-up of antiretroviral therapy in Malawi. PLoS medicine 2010;7:e1000319. ![]()
19. Compeau DR, Higgins CA. Computer self-efficacy: development of a measure and initial test. MIS Quarterly 1995;19:189–211. ![]()
20. Braa J, Macome E, Mavimbe JC, Nhampossa JL, da Costa JL, Manave A, Sitói A. A study of the actual and potential usage of information and communication technology at district and provincial levels in mozambique with a focus on the health sector. The Electronic Journal of Information Systems in Developing Countries 2001;2:1–29.
21. Källander, K, Tibenderana, J, Akpogheneta, O, Strachan, D, Hill, Z, Ten Asbroek, AH, Conteh, L, Kirkwood, B, Meek, S. Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low-and middle-income countries: a review. J Med Internet Res 2013; 15: e17.

