Mobile Phone Use and Perspectives on Tailored Texting in Adults with Diabetes
Justin Gatwood, PhD, MPH1, Rajesh Balkrishnan, PhD2, Steven R. Erickson, PharmD2, Lawrence C. An, MD3,4, John D. Piette, PhD3,5,6, Karen B. Farris, PhD2
1University of Tennessee College of Pharmacy, Memphis, TN, USA; 2University of Michigan College of Pharmacy, Ann Arbor, MI, USA; 3University of Michigan Medical School Department of Internal Medicine, Ann Arbor, MI, USA; 4University of Michigan Center for Health Communication Research, Ann Arbor, MI, USA; 5Department of Veterans Affairs Center for Clinical Management Research, Ann Arbor, MI, USA; 6Department of Health Behavior and Health Education, University of Michigan School of Public Health, Ann Arbor, MI, USA
Corresponding Author: jgatwood@uthsc.edu
Note: Portions of this article were presented at Wireless Health ’13, November 1–3, 2013, Baltimore, MD
Journal MTM 4:3:2–12, 2015
Background: Mobile phone text messaging has become increasingly popular and text-based systems for patients with chronic diseases like diabetes are being rapidly developed. A paucity of information exists about preferences for and acceptance of health-related text messages by patients for self-management support.
Aims: To evaluate the use of mobile phones, acceptance of text messaging, and perspectives on receiving tailored text messages in adults with diabetes.
Methods: A total of 48 subjects were recruited into a randomized controlled study to improve medication adherence; 21 individuals provided responses on technology acceptance and 12 semi-structured telephone interviews were conducted at follow-up. After 90 days of tailored text messages, intervention arm subjects provided feedback on acceptance of the technology, personal perspectives on the receipt of tailored materials, and preferences for mobile phone use as part of their diabetes self-management.
Results: On average, participants exchanged less than 10 messages per day and those texting more frequently tended to be younger and owned smartphones. Participants’ perception of the utility and ease of use of text messaging was positive, both of which were more positive among participants with greater perceived competence for managing their diabetes and lower perceived barriers to treatment. Subjects felt that receiving one message per day was appropriate and they benefitted from the content. In general, subjects indicated the messages were primarily useful as reminders rather than a source of new information.
Conclusions: Acceptance of tailored text messages was high in adults with diabetes and subjects felt they could benefit from receiving similar messages in the future.
Introduction
Mobile phones are now commonplace, and reflect the overall growth in wireless phone subscriptions from just over 11 million in 1992 to over 326 million in 2012.1 Currently, an estimated 91% of American adults own a mobile phone, a 78% increase from five years ago.2 Currently, most mobile devices owned by American adults are smartphones (56%), the ownership of which has increased over 20% in the past two years and penetrating all socioeconomic levels.2 A higher percentage of American adults now own mobile phones than report using the Internet.3 Moreover, while minutes of talk time have remained relatively stable, the estimated number of text messages exchanged between devices has more than doubled since 2008 to over two trillion messages in 2013.1,4
Capitalizing on connectivity, the healthcare community has begun leveraging mobile phones in the care process. As of 2012, nearly one-third of cell phone owners reported using their phone to search for health information, nearly double the number from two years before.5 Nearly one in five adults now own applications on their phone to assist in the tracking or management of health conditions.5
Considering the penetration of mobile applications and operability in the healthcare market, researchers and program developers have employed mobile technology to facilitate behavioral interventions for chronic illness self-management support. To date, text messaging has been the most popular for promoting healthy lifestyles and effective chronic disease self-care.6 Targets of these conditions have included behaviors such as smoking, appointment keeping, medication adherence, and physical activity among people with chronic diseases including diabetes, hypertension, and asthma.6–8 Medication taking has also been addressed, primarily using reminder messages to encourage medication adherence, mostly in chronic conditions.9–14
Despite these advances in mobile health service development, less than 10% of American adults receive support for disease management via text message; and less than 20% of mobile Internet usage is among adults ages 50+, i.e., those most likely to be living with chronic disease.5 However, when chronically-ill patients’ acceptance of such interventions has been evaluated, most studies have shown high levels of receptivity and satisfaction. In particular satisfaction with receiving text messages focused on medication adherence is generally high across studies evaluating interventions with a range of messaging frequencies.11,13–17 However, if mobile health interventions are to be more widely adopted, further research is needed into the use of cell phones, and their capabilities, as well as the needs and preferences in prevalent, high-risk patient populations.
Theory regarding adoption of technologies suggests that perceived ease of use and perceived usefulness (Figure 1) are both independent determinants,18,19 and both concepts are likely to play a major role in influencing chronically-ill patients’ intention to use mobile text messaging.20 While several investigations have considered the influence of external variables on perceived ease of use and usefulness, our understanding of how chronically-ill patients perceive and accept mobile messaging, in the context of healthcare delivery, is limited. In particular, factors such as patients’ age, socioeconomic class, or the complexity of their regimen may make these users’ experience different than those of healthy adults or people. Thus, a better understanding of potential factors influencing patients’ adoption and satisfaction of mobile health messages would aide practitioners and developers in improving the exchange of information with patients.
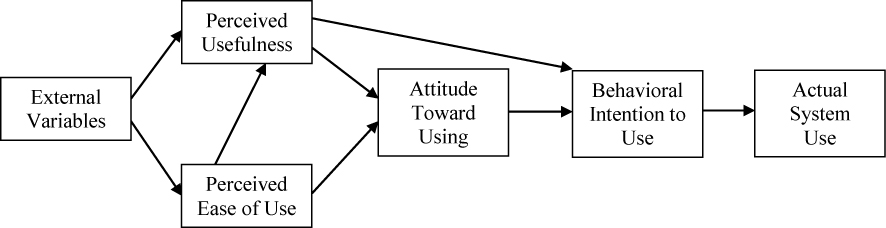
Figure 1: The Technology Acceptance Model (Adapted from Davis (1989)19)
As part of an intervention focused on improving medication adherence in adults with diabetes, the current study sought to better understand how patients use their mobile phone and in what ways they would be willing to use their phone as part of their self-management support. Here, we describe use of text messaging among adults with diabetes using anti-hyperglycemic medication. We also describe users’ responses related to the receipt of tailored text messages, and evaluate their mobile phone acceptance.
Methods
Design
Mobile phone use and acceptance in adults with diabetes was evaluated as part of a randomized, controlled intervention using tailored text messages to address antidiabetic medication nonadherence. The intervention employed theory-based, individualized text messages focused on condition and treatment-related beliefs as well as medication-specific information about efficacy, side effects, and mechanism of action over a period of 90 days with the primary intent of improving diabetes medication adherence. The message development and delivery process is described elsewhere.21 Participants in the active arm received a daily text message timed to coincide with their first medication dose; control arm subjects received a monthly “thank you” message throughout their 90-day period in addition to their standard care. Institutional Review Board approval was received from both the University of Michigan and Mercy Health Partners (Muskegon, MI) for all study components.
A total of 168 theory-driven messages and 128 medication-specific messages were developed for the study. Subjects in the intervention arm were sent a total of 2,230 messages and 94.3% were properly delivered as scheduled according to the system. Of the theory-based messages delivered, 41.4% were designed to provide encouragement (rather than reinforcement) to improve subjects’ baseline health beliefs and attitudes. Only three out of the 168 theory-based messages were not used at least once; however, more than half (55.5%) of all medication messages in the library were never used as several classes of medications were not represented.
Subjects
Participants were recruited from a community-based primary care network in western Michigan. To be eligible, participants had to be at least 21 years of age, diagnosed with diabetes, taking at least one antidiabetic medication, and have a hemoglobin A1c measured in the prior three months of at least 8.0%. Individuals were excluded if they: had experienced a stroke or heart attack, had been diagnosed with congestive heart failure, or did not own a mobile phone. Following screening and informed consent, eligible individuals were randomized to the intervention arm, in which they received one tailored text message per day for 90 days, or to standard care. All participants were mailed a baseline survey after randomization and were considered enrolled once the survey was returned. A similar survey was mailed immediately after the intervention. All participants were compensated $50 for their participation to cover the costs of receiving text messages during the study.
Subjects in the tailored text messaging arm were asked to participate in a brief phone interview (10–15 minutes) at the end of the study to capture their perspectives on the receipt of the messages. Subjects were randomly selected from the intervention cohort until half of the cohort had participated, and oral consent to participate was obtained from each interviewee prior to participating. All subjects were compensated $10 to offset the time required to be interviewed.
Data Collection
Participants’ baseline surveys included questions about their general mobile phone use and ownership (Appendix A). Among subjects in the intervention arm, technology acceptance was evaluated at follow-up (Appendix B). Four items guided by the Technology Acceptance Model were included in the endpoint survey and adapted for patients with diabetes from an instrument used to investigate SMS (text) messaging employed previously by Kim and colleagues.18,20 The included items surveyed subjects on perceived usefulness and perceived ease of use (two items for each concept), the degree of which, according to the model, influences the user’s attitude toward texting, as part of their self-care support, and their particular technology and, ultimately, their intention to use similar technology.18 Each of these items used a seven-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree). Scale reliability for perceived usefulness and perceived ease of use were 0.77 and 0.91, respectively.20 Additionally, subjects were asked about their health beliefs and level of self-determination (according to concepts related to the Health Belief Model and Self-Determination Theory) using previously validated items.21 Perceived benefit, severity, susceptibility, and barriers as well as external regulation, autonomous motivation, and perceived competence were measured using five-point and seven-point Likert scales, respectively.22–24
Questions in the telephone semi-structured interviews of intervention-group subjects focused on participants’ opinions of the text messages in terms of the messages’ content, their role in supporting self-management, whether the frequency was appropriate, and the user’s anticipated acceptance of mobile phones for diabetes management in the future (Appendix C). Interview notes were recorded on a standardized form for each response item. Electronic data were either saved on a password-protected computer or stored in a locked office within the University of Michigan College of Pharmacy.
Data Analysis
Responses to baseline survey items were combined with demographic characteristics reported by each subject and descriptively reported using t-tests or Fisher’s exact tests for continuous and categorical variables, respectively. To summarize responses for Technology Acceptance Model concepts, mean values were determined using scores from items within each concept; descriptive statistics and comparisons across demographic groups were made using Mann-Whitney tests.25 To determine whether differences in acceptance varied according to subjects’ demographic characteristics or perceptions of their diabetes self-efficacy and barriers mean values for both Technology Acceptance Model measures were compared between categorical variables by Mann-Whitney tests and among continuous variables by Spearman rank correlation.26 A key predictor of interest was users’ frequency of texting at baseline, as a measure of their acceptance of mobile technology. For analyses presented here, two groups of texters were defined, i.e., those sending or receiving no more than 10 texts per day and those who sent or received on average 11 or more per day. Annual household income was dichotomized as less than or equal to $50,000 versus higher; race was defined as White versus other race/ethnicity. Among participants from the intervention arm who participated in the endpoint interviews, responses to Technology Acceptance Model items were examined separately according to groups defined by frequency of texting and diabetes self-care self-efficacy. STATA 11.0 (College Station, TX) was used for all analyses.
Results
Subject and Mobile Phone Characteristics
A total of 400 patients were initially identified. Of those, 75 were screened for eligibility by telephone and 48 were randomized; 44 randomized patients provided outcome data at 90 days and were included in the analyses presented here. At baseline, the average age was 47 years, with half of the subjects aged 50 years and older. Nearly all subjects were Caucasian or African American, and just over half were married. Incomes tended to be higher among older participants, although there were no significant differences in income between races or genders. On average, participants reported taking two diabetes medications each day with an average of four doses per day. At endpoint, the number of medications remained unchanged but the average daily dose was slightly less (mean = 3.9, SD: 1.56). Participants in the two arms had comparable characteristics at baseline (all p >0.05). Characteristics of the intervention arm subjects are detailed in (Table 1).
Overall, two-thirds of participants reported texting 10 times or fewer per day. Among participants who texted more than 10 times per day, a significant majority (p<0.01) were 49 years of age and younger- nearly all were 39 years or younger. More frequent texting was observed in women than men (p<0.05), and texting was more frequent among smartphone users than users of basic cell phones (p<0.05). No differences in the frequency of text messaging were observed across income categories, races, or between service providers. Spending on service was no different between low and high texting subjects. At baseline, no difference in texting frequency was observed between study arms (p=0.682) and all other mobile phone characteristics were similar across arms.
Smartphones were the dominant phone type, and a majority was owned by subjects 49 years of age and younger (72%). Also, a larger share of subjects who reported annual household incomes of $50,000 or less (62%) owned smartphones. Differences in ownership of the two types of phones were not observed by race or gender.
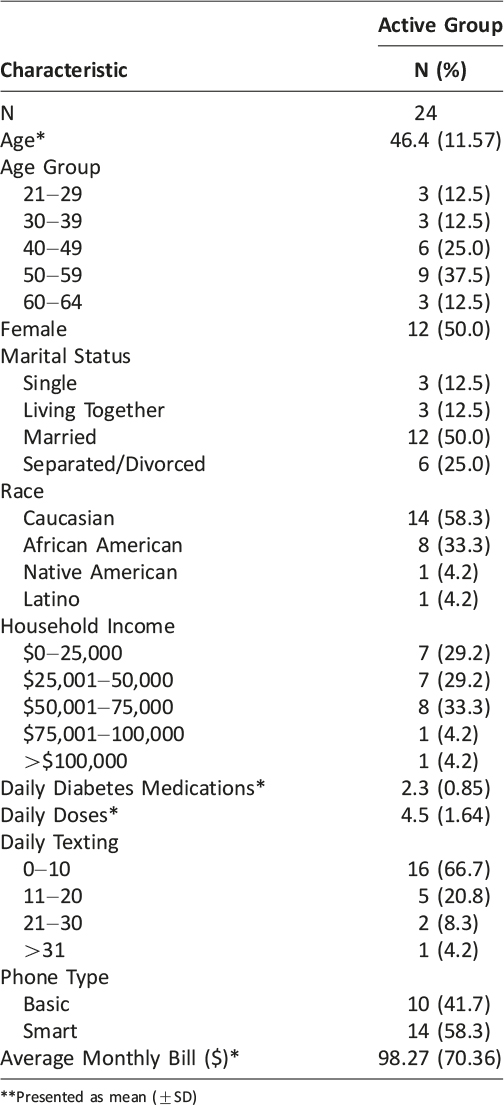
Table 1: Tailored Messaging Cohort Demographics
Technology Acceptance
By and large, acceptance was high in this population. Specifically, the mean perceived ease of use was 6.33 (SD: 0.885) and the mean for usefulness was 5.67 (SD: 1.38). Only two subjects indicated some level of disagreement to the usefulness items, and only one subject did so for the items measuring ease of use. All three of these subjects reported low daily texting, were contracted with major carriers, were male, were over the age of 50, and took their diabetes medications at least six times per day.
Among all subjects, 76% moderately or strongly agreed to both ease of use items; just over half (52%) had this level of agreement for both perceived usefulness questions. Those subjects reporting such high acceptance to all four items (42%) were similar to the characteristics of other respondents, except that they tended to be slightly older than average. No significant differences in either acceptance concepts were identified across groups defined by subjects’ demographic characteristics or types of medication regimen (oral medication alone versus insulin use). Similarly, mean values for usefulness and ease of use were comparable for subjects regardless of texting frequency and whether the participant used a smartphone (Table 2). Measures of ease of use and utility trended toward a significant relationship but did not reach statistical significance (ρ = 0.39, p=0.07). There was a trend toward significant correlation between perceived usefulness and daily doses of diabetes medications, suggesting that patients with more intensive regimens had a more positive reaction to the intervention (ρ = -0.385, p = 0.08).
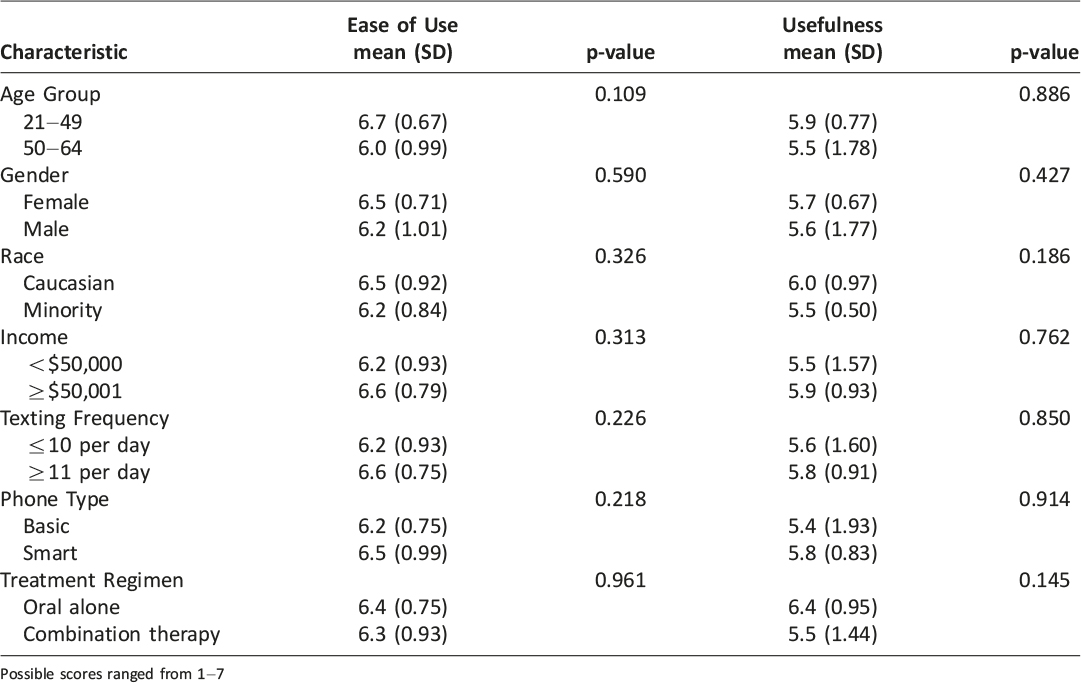
Table 2: Technology Acceptance by Category
Responses for usefulness and ease of use were also compared to patients’ responses to items measuring each of the seven health belief and self-determination concepts. Correlation analysis indicated that only ease of use was observed to have a significant relationship with other theory-driven concepts, demonstrating strong, positive association with perceived competence (ρ = 0.6, p < 0.01) and perceived barriers (ρ = 0.43, p = 0.05) to managing their diabetes self-care.
Perspectives on Treatment and Condition-Tailored Messages
Characteristics of the 12 subjects completing qualitative interviews of follow-up were generally similar to those who were not interviewed. However, interviewees were more likely to be Caucasian than non-interviewed subjects and more likely to be male (N=8). Similar to the overall sample, two-thirds reported texting 10 times or fewer per day, slightly more than half owned a smartphone, and all income categories were represented.
All but one of the subjects interviewed indicated enjoying a daily tailored text message. That remaining individual indicated that the messages were, “not worth the [additional] cost”. Subjects commonly suggested that they enjoyed the messages because they served as reminders, provided encouragement, or gave helpful tips and information. Most (9/12) reported that they found the information in the messages helpful; specific comments indicated that the information was “educational”, “encouraging”, and a “little bit of a confidence booster” or a “pep talk”. The remaining three subjects felt that the messages could have been better tailored to their specific needs or that the information provided was not relevant to their current point in treatment. One subject suggested that “[the messages] would have been more handy if [they were] based on checking sugars. I struggle with that every day. So, a reminder about sugars would have been helpful.” However, all but one person indicated that the tailoring was appropriate and that the individualization made them more likely to read and consider each message since they, “liked knowing [the message] was for me, not just generic.” Another subject noted, “I could tell they were tailored for me because they mentioned the medications I am on. Made me more likely to take them.”
In terms of the impact of the messages, a majority of interviewees (8/12) indicated that the messages made them more confident about managing their diabetes and more likely to take their medication each day (8/12). However, the most commonly mentioned motivation for taking each dose was that the timing of the message served as a reminder.
Those interviewed most commonly indicated that the messages where most helpful when the content focused on motivation, but a comparable number found medication information useful. One subject commented, “The type that gave encouragement, those ones [were the most helpful]. By remembering to take my meds like I am supposed to, I can live a longer life. Gave me encouragement to take my meds.” The messages focused on medication education were also well-received; comments included, “[I] liked the information about what your medications do, how they react, and why I should take them” and “[I] learned more about my Levemir; how it works throughout the day.” No types of messages were specifically identified as bothersome or unhelpful. All subjects indicated that it was convenient for them to receive messages by mobile phone and that receiving one message per day was sufficient. Some respondents felt the messaging dose could be individualized (e.g. additional messages to match dosing schedules) based on demand without being bothersome.
Suggestions for similar, future texting interventions varied but were generally suggestive of either increased specificity and/or the inclusion of feedback mechanisms. Participants felt that they would benefit from messages that focused on other ways to control their diabetes (e.g. diet, exercise), individualization around self-identified areas of difficulty (e.g. checking sugars), and more technical medication information. For example, one subject who was taking both short- and long-acting insulin mentioned, “I don’t know if the benefits or synergies [between the two insulin types] were discussed. A lot of programs lack giving an understanding of what the short- and long-term insulins are doing together. [I] need more messages about understanding how the medications are working together- don’t think that gets addressed.” The ability to relay information back to a provider was commonly suggested to “keep in touch with the doctor” or even find a way to receive “feedback on sugars: these were my sugars, these were my activities, my insulin doses, and recommendations on what I could do.” All but one subject indicated they would want to participate in a similar tailored messaging program if it were available in the future.
In addition to simple messaging, other functions of mobile phones that could be used for health-related purposes were mentioned; the most frequently mentioned functions were the ability to track disease progression, specifically the recording of tests and the scheduling of reminders. If subjects mentioned they would like to interact with a provider (n=8) they tended to specify this would be with their physician; however, the desire to interact with a pharmacist was indicated, “because of insurance status, especially about cost.”
Discussion
As part of a randomized controlled trial, this investigation sought to better understand the extent to which adults with diabetes use and accept mobile phone text messaging during their ongoing disease management. We found that in this population text messaging was relatively limited and younger subjects texted more frequently. Importantly, acceptance of using texting as a tool in their diabetes self-management support was high, even among older participants and those with less frequent texting. Specifically, users found the text messages user-friendly and helpful. Theoretical models about technology adoption and sustained engagement suggest that these high acceptance ratings indicate that participants would be likely to use this type of intervention in the future.18 To our knowledge, no similar diabetes texting system is currently in use as part of standard care, but these findings are encouraging in that they suggest that a similar tailored messaging system aimed at improving treatment adherence would be accepted and used. That finding is consistent with evidence from prior studies.15,16 However, as suggested in some participants’ interviews, a texting support system might be even more useful if messages were more deeply tailored to their specific treatment needs (e.g. checking sugars, lifestyle management) and the stage of therapy.
A key issue across studies of text messaging interventions focused on medication adherence has been the determination of an appropriate frequency of messaging. To date, investigations have employed a variety of such “dosing” strategies, ranging from sending messages weekly to sending messages up to 12 times per day.9,10,27 Approaches also have included varying the number of messages sent based on the subject’s specific medication dosing pattern or by stepping down the number of messages from twice daily to approximately one every other day.11,15,28 However, the most popular frequency used in text-based adherence studies has been sending one message per day.10,12–14,16 Our study found that a daily message was an appropriate level for our subjects, corroborating those earlier findings, however we also found that users would be open to variable levels of messaging as at least one other study had determined.14
Several types of messages were applied in this study, adding to our understanding of the most appropriate content for patients with diabetes. In our population, respondents’ reactions to the message content were roughly equally split between users who felt that the medication education messages were most helpful and others who found the motivational messages most useful. Respondents who preferred medication-specific messages tended to be younger and were taking more diabetes medications, and more often. Overall, this suggests that tailoring could be improved by focusing messaging on either of these two message types according to the patient’s preferences. Such an approach may then be more likely to result in positive behavior change and serve as more of a tool for motivating changes in health beliefs that drive adherence, rather than serving only as a reminder for patients who are already motivated. Interestingly, we found that participants’ perception regarding the messages’ ease of use were positively correlated with theory-driven concepts of perceived competence for diabetes self-management as well as with patients’ perceptions of the barriers to diabetes self-care. In other words, those finding text messaging relatively simple to use are also likely to be those who perceive themselves as able to successfully meet the challenge of controlling their condition and those who feel that relatively few barriers exist to effectively manage their diabetes. Future research should investigate how best to leverage mobile tools, such as text messaging, for those with a higher level of competence and with few perceived barriers to reinforce behaviors and further improve the odds of positive health outcomes. Moreover, methods should consider the impact that advanced devices (smartphones) may have on health-related behaviors and investigate the mechanisms by which text messaging and other functions built into these technologies may be leveraged to improve medication adherence and other self-management strategies.
This study was limited in several ways. The sample size for this investigation was relatively small and only some of those who participated were surveyed on technology acceptance and interviewed to obtain their personal perspectives about the intervention. While the responses provide guidance on how adults with diabetes use their mobile phones and how text messaging studies may be structured, the views reported may not be representative of the general population of adults with diabetes. Additionally, only a limited set of messages was sent to the subjects throughout the study; the mix of messages may have influenced the usefulness of the messaging program. Furthermore, the subjects recruited could also have had either type 1 or type 2 diabetes and may have had their condition for any number of years; however, the messages were not drafted with either type of diabetes or stage of treatment in mind. The intervention also assumed that individual medication regimens were the same throughout the three months of the study. While only three subjects within the intervention arm reported a change in medications over the 90-day period, the inability to alter medication messages after baseline limited the extent to which these messages could have been tailored, resulting in some inappropriate messaging for those placed on a new medication. Finally, while the system used to deliver the messages was able to confirm that the messages reached participants’ phones, we could not confirm that each message was read.
Conclusions
This study found that adults with diabetes are accepting of text messaging as a tool for assisting them with self-management. Daily messages focused on behavioral motivations, health beliefs, or medication education were generally viewed as appropriate. The use of a similar intervention may benefit adults with diabetes or other chronic conditions, and future investigations should evaluate how best to leverage tailored material delivered by mobile phones. Next generation interventions should consider individual patient preferences in terms of messaging content and dose, the relaying of feedback, and direct communication between patients and providers in order to improve patient engagement and the impact of these services on health outcomes.
Acknowledgements
The study authors wish to thank Jason Barnum, PharmD (Mercy Health Partners) for his assistance with identifying potentially eligible subjects and Katie S. Kaminski, PharmD (University of North Carolina Hospitals) for her assistance with recruiting subjects for the intervention. We are also grateful for the financial assistance provided by the University of Michigan Rackham Graduate School and the supporting funding from the Agency for Healthcare Research and Quality through grant number HS021976 (R36). John Piette is a VA Senior Research Career Scientist. Additional financial support came from grant number P30DK092926 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Funding
Support for this research was provided by AHRQ grant number HS021976 (R36) and the University of Michigan Rackham Graduate School.
Disclosure
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: support from the Agency for Healthcare Research and Quality and the University of Michigan for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
References
1. CTIA- The Wireless Association. Semi-annual wireless industry survey. 2013. Online. Available at: http://www.ctia.org/advocacy/research/index.cfm/aid/10316.
2. Pew Research Center. Smartphone ownership—2013 Update. June 5, 2013. Online. Available at: http://www.pewinternet.org/Reports/2013/Smartphone-Ownership-2013.aspx
3. Pew Research Center. Internet adoption, 1995-2013. 2013. Online. Available at: http://www.pewinternet.org/Static-Pages/Trend-Data-(Adults)/Internet-Adoption.aspx
4. Pew Research Center. American and Text Messaging. September 19, 2011. Online. Available at: http://www.pewinternet.org/Reports/2011/Cell-Phone-Texting-2011.aspx
5. Pew Research Center. Mobile Health 2012. November 8, 2012. Online. Available at: http://www.pewinternet.org/Reports/2012/Mobile-Health.aspx
6. Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E-Health 2009;15:231–40. ![]()
7. Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med 2009;36:165–73. ![]()
8. Wei J, Hollin I, Kachnowski S. A review of the use of mobile phone text messaging in clinical and healthy behaviour interventions. J Telemed Telecare 2011;17:41–8. ![]()
9. Marquez-Contreras E, Figuera von Wichmann M, Guillen V, et al. Effectiveness of an intervention to provide information to patients with hypertension as short text messages of reminders sent to their mobile phone. Atencion Primaria 2004;34:399–405. ![]()
10. Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS 2011;25:825–34. ![]()
11. Vervloet M, van Dijk L, Santen-Reestman J, et al. SMS reminders improve adherence to oral medication in type 2 diabetes patients who are real time electronically monitored. Int J Med Inform 2012;81:594–604. ![]()
12. Cocosila M, Archer N, Haynes RB, et al. Can wireless text messaging improve adherence to preventive activities? Results of a randomized controlled trial. Int J Med Inform 2009;78:230–8. ![]()
13. Hou MY, Hurwitz S, Kavanagh E, et al. Using daily text-message reminders to improve adherence with oral contraceptives, a randomized controlled trial. Obstet Gynecol 2010;116:633–40. ![]()
14. Strandbygaard U, Thomsen SF, Backer V. A daily SMS reminder increases adherence to asthma treatment: A three-month follow-up study. Resp Med 2010;104:166–71. ![]()
15. Hardy H, Kumar V, Doros G, et al. Randomized controlled trial of a personalized cellular phone reminder system to enhance adherence to antiretroviral therapy. AIDS Patient Care STDs 2011;25:153–61.
16. Franklin VL, Waller A, Pagliarit C, et al. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med 2006;23:1332–8. ![]()
17. Arora S, Peters AL, Agy C, et al. A mobile health intervention for inner city patients with poorly controlled diabetes: Proof-of-concept of the Text-MED Program. Diab Tech Ther 2012;14:492–6. ![]()
18. Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly 1989;13:319–40. ![]()
19. Davis FD, Bagozzi RP, Warshaw PR. User acceptance of computer technology: A comparison of two theoretical models. Manag Sci 1989;35:982–1003. ![]()
20. Kim GS, Park S, Oh J. An examination of factors influencing consumer adoption of short message service (SMS). Psychology & Marketing 2008;25:769–86. ![]()
21. Gatwood J, Balkrishnan R, Erickson SR, et al. Addressing medication nonadherence by mobile phone: Development and delivery of tailored messages. Res Social Adm Pharm 2014; ![]() .
.
22. Becker MH, Janz NK. The Health Belief Model applied to understanding diabetes regimen compliance. Diabetes Educator 1985;11:41–7. ![]()
23. Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care 1998;21:1644–51. ![]()
24. Williams GC, Freedman Z, Deci EL. Promoting motivation for diabetics’ self-regulation of HbA1c. Diabetes 1996;45:13A.
25. Fay MP, Proschan MA. Wilcoxon-Mann-Whitney or t-test? On assumptions for hypothesis tests and multiple interpretations of decision rules. Stat Surv 2010;4:1–39. ![]()
26. Cohen J, Cohen P, West SG, et al. Applied multiple regression/correlation analysis of the behavioral sciences. 3rd ed. Mahwah, New Jersey: Lawrence Erlbaum Associates; 2003.
27. Granholm E, Ben-Zeev D, Link PC, et al. Mobile assessment and treatment for schizophrenia (MATS): A pilot trial of an interactive text messaging intervention for medication adherence, socialization, and auditory hallucinations. Schizophr Bull 2012;38:414–25. ![]()
28. Petrie KJ, Perry K, Broadbent E, et al. A text message programme designed to modify patients’ illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psych 2012;17:74–84. ![]()
Appendix A: Mobile Phone Use Survey
The following 4 questions relate to your use of mobile phone text messaging. If you own and operate more than one mobile phone, please answer them based on your primary phone only. If you do not know exact numbers, please estimate as best as possible. Place your answer in the space provided.
- 1. In a typical day, how many text messages do you send and receive?
_____1–10
_____11–20
_____21–30
_____31 or more
- 2. What best describes the type of phone you own?
_____Smartphone
_____Basic phone
- 3. To which of the following service providers do you subscribe?
_____Verizon
_____AT&T
_____Sprint
_____T Mobile
_____Cricket
_____MetroPCS
_____Other
- 4. On average, what is your monthly bill for mobile phone services?
$________________
_____Don’t know
Appendix B: Technology Acceptance Survey Items
- 1. Using text messaging as part of my diabetes treatment increases my chances of achieving things that are important to me.
- 2. Using text messaging as part of my diabetes treatment helps me accomplish things more quickly.
- 3. I think learning how to use text messaging as part of my diabetes treatment is easy for me.
- 4. I find text messaging as part of my diabetes treatment easy to use.
Appendix C: Intervention Exit Interview Items
- 1. Did you enjoy receiving messages on your phone specific to your condition and treatment?
a. Yes: What specifically did you enjoy?
b. No: Why were these messages not enjoyable to receive?
i. Potential follow-up: Was this due to the content of the message?
ii. Potential follow-up: Was this because it was received on your phone?
- 2. Did you find the information in these messages helpful in your ongoing treatment?
a. Yes: What did you find most helpful?
b. No: Why do you feel these messages were not helpful?
- 3. You received several types of messages over the course of these 3 months. Could you describe the ones that you found to be the most helpful, interesting, or educational?
- 4. Similarly, could you also describe the types of messages you found to be the most distracting, unhelpful, or bothersome?
- 5. If you were to continue to receive messages on your phone about your treatment and/or condition, what topics or material should these messages focus on?
- 6. You received one message each day for 90 days. Was this too much, too little, or about right?
a. Potential follow-up: How often and how many messages would you prefer to receive?
- 7. Was it convenient for you to receive these messages on your phone?
a. Yes: Is this your preferred method of receiving health-related information?
b. No: How else would you prefer to receive health-related information? (Suggested sources: online, e-mail, mail.)
- 8. The messages you received were created specifically for you, meaning they were tailored to your treatment and current condition. Did this make you more or less likely to read, consider, and act on each message?
- 9. After receiving these messages for 90 days, do you feel more confident about managing your diabetes than you did before the study began?
- 10. When you received these messages did it make you more or less likely to take your prescribed medication for the day?
a. Yes: What made you more likely to do so?
b. No: What aspect of the messages made you less likely to do so?
- 11. In the future, how could we make a message-based system, similar to this one, more effective in terms of providing individual information and support? (Suggested topics: types of messages, interaction, timing.)
- 12. In the future, would you consider receiving tailored messages on your phone throughout the course of your treatment, similar to what you have for the past 3 months?
- 13. After receiving health-related information on your phone for 90 days, how likely are you to use your mobile phone for other health-related activities, such as tracking your condition, interacting with a healthcare provider, or looking up information?

