Application of mobile technology in ophthalmology to meet the demands of low-resource settings
Dr Rahul Chakrabarti MBBS1,2
1 Editor-In-Chief, Journal of Mobile Technology in Medicine, 2Centre for Eye Research, Australia
Corresponding Author: rahul@journalmtm.com
Journal MTM 1:4:1-3, 2012
DOI:10.7309/jmtm.70
The capacity for mobile technology to play an important role in facilitating patient care in low-resource settings was evidenced by the recent 9th General Assembly of the International Agency for Prevention of Blindness (IAPB) held in Hyderabad, India. Amongst the major priorities emphasised by the Vision 2020 consortium was the goal to provide universal coverage and access to services to preserve sight. Fundamental to achieving this target was the need to strengthen health systems by development and provision of accessible and affordable health technology.1 The conference theme was ‘eye care – it’s everyone’s business’, exhibited excellent examples of innovation and scientific rigour in the application of telemedicine and mobile health in the field of ophthalmology.
One area where the advent of telemedicine has demonstrated greatest benefit is in the provision of ophthalmic services to address the growing demands of non-communicable (NCD) diseases. In the field of diabetic retinopathy (DR) screening and management, the Aravind Eye Care system based in Madurai, India demonstrated that an ‘Advanced Eye Screening Unit’ in a mobile van was capable of performing community outreach to identify DR. In their model, a non-mydriatic retinal camera was used by a trained technician to acquire retinal photographs that were stored and sent via satellite internet to a central reading and grading centre at the tertiary ophthalmic facility, where “live” grading was performed and feedback communicated to the mobile van.2 A similar approach has been developed by the LV Prasad Eye Institute (LVPEI) based in Hyderabad whereby patients with diabetes presenting to a diabetes clinic in a rural area received dilated retinal photography by a trained photographer.3 Images were then transferred via cable internet network to a consulting retinal specialist at the tertiary ophthalmic facility in Hyderabad who graded the image and advised on appropriate management. The advantages of both these models were that the consulting ophthalmologist was “online” at the time when the photographs were taken. This enabled a turnover of approximately ten minutes between patient presentation and diagnosis.
Clearly, there are several challenges to implementing such screening systems in other low-resource settings. In South Africa, Mash et al conducted a pilot study of non-mydriatic retinal photography performed at a community facility for patients with diabetes. The authors highlighted that affordability of reliable photographic software and access to a fast and secure internet network to transfer images were critical barriers to sustainability of the service.4 Another obvious barrier is cost of equipment. Current non-mydriatic retinal cameras are expensive (ranging up to USD$20,000) and are limited in their ‘field-readiness’ parameters including portability, training requirements, and degree of difficulty of use.5 Whilst newer generation non-mydriatic retinal cameras are commercially available6 with features including wireless network connection, validation studies of such devices are yet to be published and they remain expensive. This has prompted several groups to consider alternative and more affordable and accessible technologies in ophthalmology.
One innovation that gained particular interest at the IAPB conference was the development of the world’s smallest and most versatile ophthalmoscope and otoscope, the ‘Arc-Light’ scope. (See Figure 1) This device was developed and patented by the University of Leicester. Shaped to conveniently fit in a pocket, the device weighs 18 grams, consists of 4 magnification settings (+4, 0, -3,-6 dioptres) and a 3x loupe for magnification to which an otoscope ear piece can be attached. The Arc-Light is powered by an integrated solar panel (duration of 2-3 hours), and also has a USB port that enables it to be charged from a computer or compatible mobile phone. The developers also incorporated a pupil gauge, ruler, near visual acuity chart, colour test and 3 intensity level LED bulbs. Anecdotal evidence has demonstrated the capacity for clinical photographs of cornea and anterior chamber of the eye to be acquired through the ophthalmoscope. However, it is yet to be determined whether the instrument is as accurate and easy compared to the direct ophthalmoscope and non-mydriatic retinal camera for the purposes of retinal examination. Whilst validation studies are presently in progress, at a market cost of US$10, it is logical that such devices will be rapidly disseminated to primary health care and village health facilities where retinal cameras are not readily affordable.
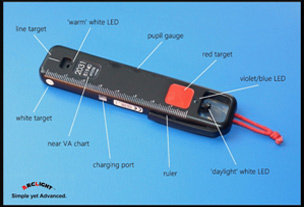
Figure 1. The Arc Light ophthalmoscope. Image courtesy of : Arclight-scope.com
The versatility of smartphones to aid clinical assessment has been shown in several recent publications. In the previous issue of this journal and also at the IAPB conference, Bastawrous et al demonstrated the ability for refraction to be assessed using a pinhole adaptor to an iPhone.7 The authors showed there was no statistically significant difference in the Near Eye Tool for Refractive Assessment (NETRA) adaptor compared to standard subjective assessment of a patient’s refraction (spherical equivalence). Additionally, at a market price of USD$30, it demonstrated the potential for such innovations to be cost-effective particularly in low resource settings where optometrists or trained refractionists are not readily available.

Figure 2. The smartphone slit-lamp adaptor. Image courtesy of eyewiki.aa.org
Smartphones have also been explored as adjuncts to clinical examination for ophthalmic pathology. Commercially available slit-lamp adaptors have been demonstrated to be able to capture adequate quality imaging of the anterior chamber of the eye.8 Lord et al have previously described retinal
imaging using an iPhone and indirect lens.9 However, the sensitivity and specificity for imaging posterior segment disease using this technique is yet to be validated. More recently, Lamirel et al demonstrated that retinal images taken using a non-mydriatic camera in an emergency department setting were able to be transferred and graded by an off-site ophthalmologist with high accuracy on an iPhone display to identify emergent retinal and optic disc pathology.10 Given that smartphone cameras have an ever increasing image resolution it is conceivable that in the near future smartphones may provide fundus images to facilitate early referral of patients in low-resource settings.
From these examples in the field of ophthalmology, it is clear that advances in telemedicine and validation of smartphone technology will improve access to eye care worldwide. The greatest benefit will be in low and low-middle income countries where a major challenge is the provision and accessibility of trained eye-care professionals. Further validation studies of these novel devices will be an important next step for enhancing the role of mobile health to provide timely diagnosis and treatment for underserved populations.
References
1. WHO. Action plan for the prevention of avoidable blindness and visual impairment, 2009-2013. Geneva: World Health Organisation;2010.
2. Perumalsamy N, Prasad NM, Sathya S, Ramasamy K. Software for reading and grading diabetic retinopathy: Aravind Diabetic Retinopathy Screening 3.0. Diabetes Care. Sep 2007;30(9):2302-2306. ![]()
3. Rao GN, Khanna RC, Athota SM, Rajshekar V, Rani PK. Integrated model of primary and secondary eye care for underserved rural areas: The L V Prasad Eye Institute experience. Indian J Ophthalmol. Sep 2012;60(5):396-400. ![]()
4. Mash B, Powell D, du Plessis F, van Vuuren U, Michalowska M, Levitt N. Screening for diabetic retinopathy in primary care with a mobile fundal camera–evaluation of a South African pilot project. S Afr Med J. Dec 2007;97(12):1284-1288.
5. Friedman DS, Ali F, Kourgialis N. Diabetic retinopathy in the developing world: how to approach identifying and treating underserved populations. Am J Ophthalmol. Feb 2011;151(2):192-194 e191.
6. Volk. Volk Pictor. 2011; http://volk.com/catalog/index.php?cPath=53. Accessed 20/9/2012.
7. Bastawrous A, Leak C, Howard F, Kumar B. Validation of a Near Eye Tool for Refractive Assessment (NETRA)- Pilot Study. Journal of Mobile Technology in Medicine. 2012;1(3):6-16. ![]()
8. Bastawrous A, Cheeseman RC, Kumar A. iPhones for eye surgeons. Eye (Lond). Mar 2012;26(3):343-354. ![]()
9. Lord RK, Shah VA, San Filippo AN, Krishna R. Novel uses of smartphones in ophthalmology. Ophthalmology. Jun 2010;117(6):1274-1274 e1273.
10. Lamirel C, Bruce BB, Wright DW, Newman NJ, Biousse V. Nonmydriatic Digital Ocular Fundus Photography on the iPhone 3G: The FOTO-ED Study. Arch Ophthalmol. Jul 1 2012;130(7):939-940. ![]()

