mHealth intervention development to support patients with active tuberculosis
Sarah J. Iribarren, PhD1,2, Susan L. Beck, PhD, APRN, FAAN, AOCN2, Patricia F. Pearce, MPH, PhD, APRN, FAANP, FANP3, Cristina Chirico, MPH, MD4, Mirta Etchevarria4, Fernando Rubinstein, MPH, MD5
1Columbia University School of Nursing, New York, NY, USA; 2University of Utah, College of Nursing, Salt Lake City, UT, USA;
3School of Nursing, Loyola University, New Orleans, LA, USA; 4Region V TB Program, Province of Buenos Aires, Argentina;
5Institute for Clinical Effectiveness and Healthcare Policy, Buenos Aires, Argentina
Corresponding author: si2277@cumc.columbia.edu
Journal MTM 3:2:16–27, 2014
Background: Mobile Health (mHealth) based interventions have been increasingly used to improve a broad range of health outcomes. However, few researchers have reported on the process or the application of theory to guide the development of mHealth based interventions, or specifically for tuberculosis (TB) treatment management.
Aims: To describe the steps, process, and considerations in developing a text messaging-based intervention to promote treatment adherence and provide support to patients with active TB.
Methods: Traditional qualitative techniques, including semi-structured interviews, field notes, content analysis, iterative coding, and thematic analysis, were used to design and document the intervention development with a multidisciplinary team of researchers, clinicians, administrators, and patients who were in active TB treatment. The Information-Motivation-Behavioral Skills (IMB) model was used to guide the coding scheme for content analysis of patient-directed TB educational material and intervention development.
Results: The development steps included: a) establishing intervention components, including justifications, considerations, timing and frequency of components; b) developing educational messages, including cultural adaption, text or short message service (SMS) formatting, and prioritizing message delivery order; and c) determining implementation protocol. A set of 16 IMB-based messages were developed for the educational component. Final intervention development was achieved in 3 months.
Conclusion: A collaborative approach and application of a theory to guide the intervention design and development is supported. Although a collaborative approach was more time consuming, it resulted in a more responsive, culturally appropriate, and comprehensive intervention. Considerations for developing a text messaging based intervention are provided and may serve as a guide for similar interventions. Further empirical evidence is needed for applying the IMB model for adherence-promotion in TB efforts.
Introduction
Text messaging or short message service (SMS) has been applied to an array of mobile health (mHealth) based interventions.1,2 However, few researchers have reported on the process or the application of theory to guide SMS-based intervention development.3 Furthermore, although a promising tool to improve tuberculosis (TB) treatment adherence,4 there has been little research applying it to TB management.5
The SMS mobile phone feature is commonly used, more economical than a phone call, can be sent, stored, answered, and retrieved at the user’s convenience, and is accessible with nearly the global population reported as having a mobile phone.6 Although communicating or providing information through SMS may improve efficiency, it does present unique challenges compared to face-to-face or paper-based exchange of complex information.7 When developing messages the style, language, and length of text must be considered.8 In addition, many researchers have used SMS to send reminders for adherence,9–15 but fewer have described using its interactive feature.5,16 End users and clinicians should participate in intervention development.3 The purpose of this paper is to describe the early stages of a collaborative process to develop an SMS-based intervention in Argentina where TB treatment success rates have remained consistently low17 and about half of the patients receive treatment by self-administration.18 Rationale for decisions and considerations for the intervention development and specific steps for SMS adaption are described along with a novel approach to applying the Information-Motivation-Behavioral Skills (IMB) model.19,20
The IMB model, initially developed to promote HIV prevention interventions in inner-city minority settings,21,22 also provides a model to promote adherence to treatment.19,20 The model supports the hypothesis that to initiate and maintain a desired behavior, such as medication adherence, adherence-related information and motivation must be provided, along with appropriate tools and strategies to maintain the behavior.19 Adherence-related information should target information gaps and focus on delivering accurate information regarding disease, its treatment and transmission, and medication side effects or drug interactions.19,20 Motivation can be strengthened by focusing on beliefs and attitudes towards adherence and by providing social support or social norms for engaging in behavior change. The IMB model has been suggested as a promising theoretical model to promote active TB medication adherence,20 but has yet to be applied and tested as such. In TB literature the model has been applied to guide researchers to assess healthcare workers TB infection control information, motivation and behavior skills23 and to suggest examples of ways to manage latent TB.24
The process described in this paper was part of a larger study that examined the feasibility and acceptability of the developed intervention and further assessed patient input.25 Information provided can help guide future development of similar SMS-based interventions and provides key steps and recommendations.
Methods
Traditional qualitative techniques,26–28 including semi-structured interviews, field notes, content analysis, iterative coding, and thematic analysis, were used to design and document the intervention development with a multidisciplinary team of researchers, clinicians, administrators, and patients who were in active TB treatment. The multidisciplinary team (hereafter called the team) consisted of: a regional TB director/pulmonologist, the lead regional TB social worker, a regional TB technician, two TB-specialized clinical nurses, and the hospital TB program director/pulmonologist. The regional TB director was involved from the beginning of the initial drafting of the research proposal. Five patients in active TB treatment participated in the educational message component development. The patients were individually interviewed by the primary investigator (PI) and a clinical nurse regarding the type of information/education they would have liked to have known or received during the first phase of treatment, what concerns or doubts they had regarding diagnosis or treatment, and what they would recommend to include in educational messages that could help others complete treatment. The team reviewed the overall study objectives and participated in development of the intervention through virtual and in-person meetings. Educational content was adapted based on use for SMS through an iterative process to meet character count limit, provide clear and concise educational messages, and incorporate the IMB model components. A daily study log and field notes were maintained to document the process of intervention development. We then piloted the intervention with patients initiating active TB treatment by self-administration.25 This research was approved by the Institutional Review Boards of the University of Utah and an independent research ethics board of Hospital Italiano, in Argentina.
Setting
This study was completed in the outpatient clinic at a public pulmonary-specialized regional reference hospital in the province of Buenos Aires, Argentina. The regional hospital served a large geographic region with a population of 3.5 million and accounted for one quarter of the TB cases within the province.29
Educational Content Selection
The PI conducted a content analysis of patient-directed TB educational material prior to patient and expert input. The goal of the content analysis was to produce a list of educational message options based on the IMB model to help guide content development. The PI adapted the IMB model19,21 for TB treatment adherence (see Fig. 1) and developed a coding scheme27,28 based on the model (see Table 1) to code patient-directed educational material.
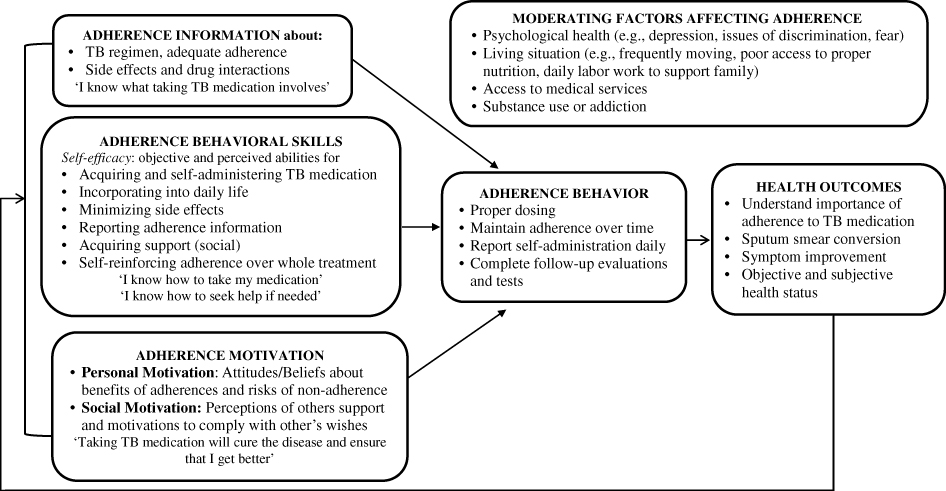
Figure 1: Information-Motivation-Behavior Skills model of TB adherence. Adapted from Fisher et al. 2006 and Munro et al. 2007
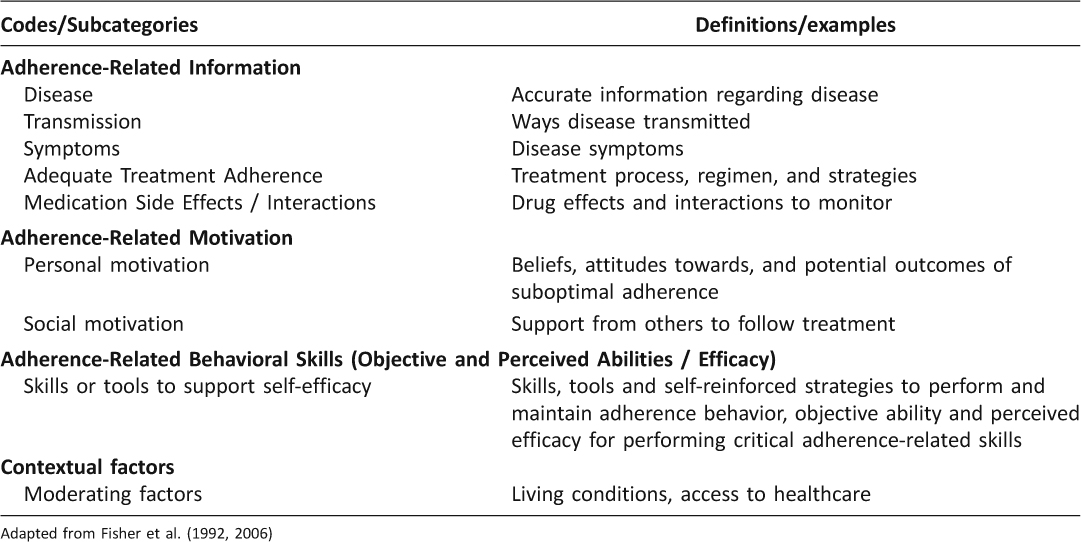
Table 1: Coding Scheme Based on IMB Model: Codes and Definitions
To identify patient-directed TB educational material the PI conducted online searches without a date limit in December, 2011, using search terms tuberculosis and patient education. Primary/major websites accessed included the World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), and secondary searches into specific institutes or university centers (e.g., UCSF), state public health departments (e.g., Minnesota and Virginia Department of Health). Searches were also conducted for HIV/AIDS patient education to identify IMB-based language that could be adapted to TB patient education. Relevant material was considered: written for patients as the target audience, accessible on-line and including information on active TB. Excluded were materials not pertinent for patients diagnosed with active TB (e.g., how it is diagnosed, treatment for latent TB infection), and graphics and photos because they may be more challenging to use in text messages or may not be received by all phones. Searches were conducted until no new material was found. To facilitate the translation process, Spanish versions of the educational material were collected when available. The educational material was compiled and coded based on the coding scheme. The unit of analysis was a complete education message summarized in one to two sentences. Similar or duplicate messages were deleted. ATLAS.ti version 6 (GmbH, Berlin, 2009) was used for data analysis support and organization. A TB specialist manual,30 WHO recommendations,31 and local patient TB educational material were also used to identify material and crosscheck messages.
Results
The following describes decision making steps for: a) establishing intervention components, including justifications, considerations, timing and frequency of components; b) developing educational messages, including cultural adaption, SMS formatting, prioritizing message delivery order; and c) determining implementation protocol. Table 2 provides English translated examples of the educational messages. Table 3 outlines the key recommendations and examples specific to developing a text messaging based intervention.
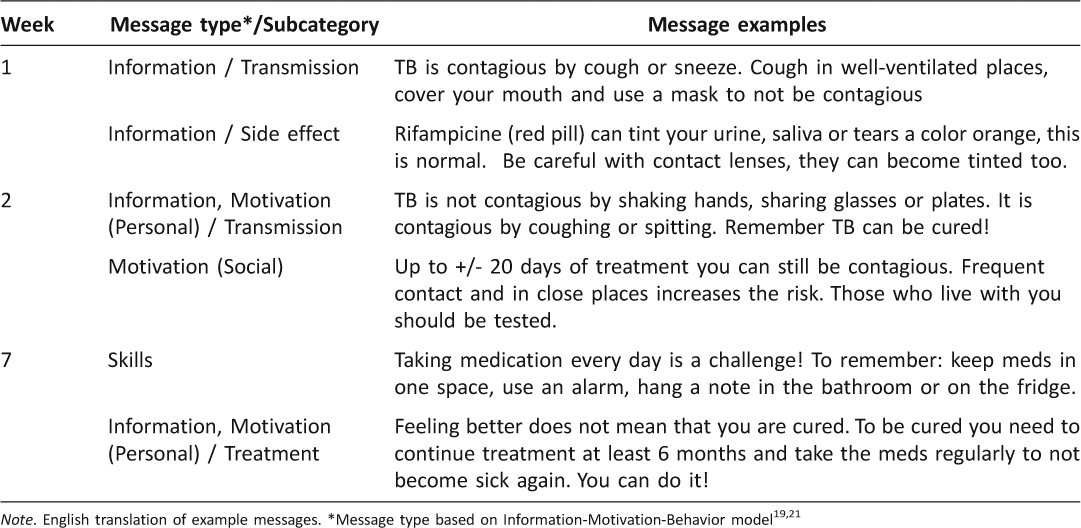
Table 2: Examples of SMS Educational Messages: Week Delivered, Type and Message Examples
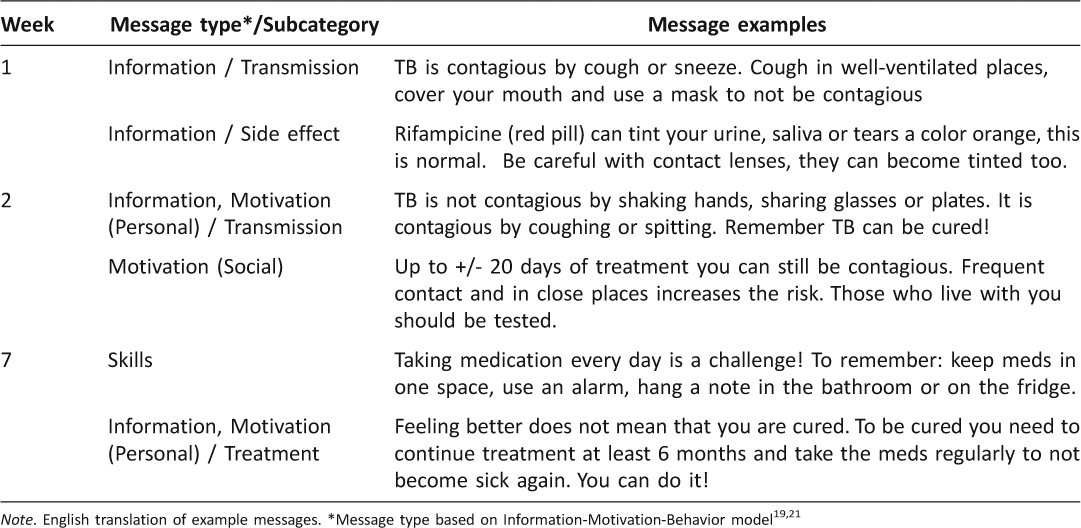
Table 3: Key Recommendations and Examples Specific to Designing SMS-based Interventions
Establishing Intervention Components
The basis for having the patient text-in was to increase patient involvement in their care. The team wanted patients to be responsible for reporting with follow-up reminders being sent only to those who did not text-in. An option for patients to text-in questions and a process for verifying receipt of text-in notification by sending a confirmation message were added. In addition, the team decided on sending two educational text messages per week. TextTB was coined by a team member and agreed upon to give the program a name. Final intervention components are outlined in Figure 2.
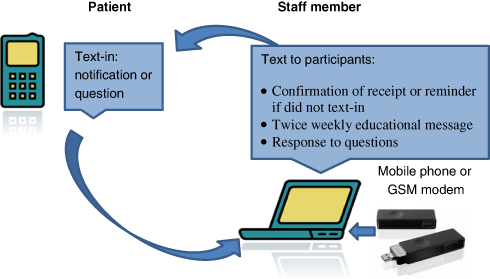
Figure 2: Intervention components
Dosing for TB medication is daily. However, because the clinic was closed on weekends the decision was made that texting-in on weekends or holidays was optional. Participants were notified that the service was only available during office hours. Educational text messages were delivered on Tuesdays and Thursdays because most holidays fell on Mondays and Fridays.
It is recommended that TB medication is taken while fasting, or in the morning, before eating, for best effectiveness.30 Therefore, the team decided that messages would be reviewed and responded to starting around 9:00 am and throughout the clinic hours of operation to identify those who had not texted in and send out query texts. With the texting platform used, this process could not be automated. A set of possible inquiry message options was written that could be modified or personalized. It was recognized that phone signal coverage, power outages, and other problems may be a potential barrier to send or receive messages. The first step was to send messages of inquiry. These messages were written to not be accusatory, but to recognize that other possible challenges may have occurred. For example, “We know that you normally take your medication and notify daily but today we have not yet received notification, any problems?” (English translation).
The process to send a confirmation message of receipt of texting-in could be automated by setting keywords. A concern of the team was that the intervention should not be what was labeled too automated. That is, messages could not be too repetitive, and needed to be creative and motivating based on the IMB model to engage participants. A list of confirmation messages incorporating motivational elements were produced to rotate automatic messages (e.g., “Thank you for your collaboration; you are doing great keep it up”! (English translation)).
Developing Educational Text Messages
Education regarding TB treatment was identified by the patients and team as often lacking during diagnosis and treatment delivery and therefore was considered a critical component of the intervention. For the educational message content selection we prioritized the information provided by the patients and that which was considered important by the team members. Patients recommended including content on: (a) nutrition during treatment, (b) what to do when feeling bad (e.g., side effects–seek help from provider), (c) effects of medication over time (e.g., often side effects pass and it gets easier), and (d) acknowledgement that the treatment is challenging (e.g., that there are a lot of pills to take every day and for a long period). Specific English translated messages patients recommended to include in educational content included: “Continue, it is worth the effort to continue treatment,” “If you feel bad go to the doctor so you can continue treatment,” and “you are going to have a stomach ache but this will pass.” Some of the necessary content topics identified by the team included: medication and food interactions (e.g., interaction of TB medication with oral contraceptives for women), important time periods (e.g., when to return for follow-up), contact testing (e.g., having family and close contacts tested), and continue to take the medication even after feeling better.
The analysis of the patient-directed TB education material resulted in 145 verbatim educational content options organized into each of the IMB model categories. The compiled list of educational content options was given to the team to review during content development. We reviewed the recommendations/priorities from the patients and the team, the list of educational content options, and other resources until 16 messages (two per week for 2 months) were identified. Messages were not taken verbatim from any of the sources. Having content options organized according to the IMB model allowed selection from each category or a combination. Content on food and medication interactions, recommended to be included by patients and team, was not found in the patient education material and was drawn from a TB provider manual.30
The HIV/AIDS patient education material was compiled, coded, and analyzed based on the coding scheme as well to explore IMB-based language that could be adapted to TB education. For example, statement of “You are not alone” in HIV material, was not identified in TB education material. In addition, pronoun use of ‘we’ rather than ‘you’ was significantly higher in HIV/AIDS patient education (p=0.001) than in TB patient directed education.
Once we decided on a list of messages, which included patient and team topic recommendations and incorporated aspects of the IMB model using the list of message options, we then culturally adapted and formatted the messages. During the Spanish translation/cultural adaptation process the team decided on using the informal conjugation of you rather than the formal conjugation, so that the messages were more personal. In general an SMS is limited to 160 characters. Common word abbreviations were identified to accommodate more text, and to be clear and concise to meet the character limit. Examples of abbreviations included: please (por favor) abbreviated as X; and that, what (que) abbreviated as q or k. In addition, the team decided to omit object pronouns (e.g., el, la, los, las) where possible. The process to reduce and distill the messages was time consuming and required many iterations. Table 2 provides examples of English translated messages, the IMB component they were classified under, and the week of treatment they were delivered.
Another cultural adaptation included team members identifying that the baseline demographic and TB knowledge questionnaire (pre-intervention survey) required local Spanish language adaptation. Although the questionnaire was correctly translated by a native Spanish speaker from Mexico, it needed to be adapted to Argentinian Spanish. Team members also requested removal of the question on race/ethnicity because it is a question not understood or requested standardly from Argentineans.
Prioritizing message delivery order was an important consideration. For example, shortly after starting one of the TB medications, rifampin, the color of urine can change to reddish orange, which can be frightening for those who are not forewarned that this is a normal, harmless side effect of the medication. Another prioritized initial message was regarding encouraging the patient to have family members or close contacts be tested for TB in order to detect infection early and help prevent further spread of the disease. Important time points identified by the team were at 1 and 2 months of treatment when follow-up with their provider was needed to evaluate treatment progress and are times recognized as susceptible to treatment abandonment because patients often start feeling better. Messages to reinforce follow-up visits and to continue medication even after a period of seeming recovery were scheduled to be delivered at these time points.
Determining Implementation Protocol
The need for materials for participants, daily operating procedures and anticipatory guidance were identified. Written information to accompany verbal instructions for participants in the intervention was developed into an instructional pamphlet which included key goals, expectations of the patient, the study phone number, and examples for how to text-in to report daily medication administration. The team developed daily operating procedures and the PI integrated the procedures into a formal document. Operating procedures included steps to initiate SMS software and modem set-up, established times to review and respond to messages, documentation of patient tracking, and intervals to review patient and modem phone credit.
Discussion regarding decision points for such instances as a participant not texting-in to report medication administration initiated an algorithm design. If there was no response the patient would receive inquiry messages for 3 days and the team member would attempt to call. If contact could not be made the staff would notify the nurse and social worker. The social worker would attempt to contact the healthcare center close to the patient to see if the patient could be tracked down locally. The RNs would notify the staff if the patient came in to the clinic in order for staff to speak with the patient directly to identify challenges with notifying by SMS.
Discussion
Although a number of researchers report applying SMS-based interventions to promote behavior change,2,14,15,32 few have described the process of development. This research adds to existent knowledge about collaborative research emphasizing text messaging intervention development for patients with active TB. Decision making justifications, considerations, and integration of a theoretical model to guide message content selection is outlined. This paper parallels similar information from Gold et al.8 and Owens et al.3 collaborative work to include service users, participants, and clinicians, but extends these contributions to present process detail for message development and planned implementation of an SMS-based intervention.
Person and colleagues found that patients attending TB and HIV clinics were generally receptive to text messaging for healthcare-related communication.33 However, identified mobile phone-related TB studies have used the video feature34–36 and no studies were identified to use SMS to deliver TB educational messages. To date, published literature of larger studies using SMS has focused on antiretroviral therapy adherence for patients with HIV/AIDS, including sending a text message asking “how are you?”37 and sending automatic text medication reminders.12,14 A study protocol outlined how researchers proposed to use reminders with a motivational message,38 but do not describe how the motivational messages were designed.
Contextual Appropriateness and Potential to Provide Patient Support
Mobile phones are increasingly relevant in resource-limited settings and incorporating their use has been identified as a priority by the WHO.39 In the current research, the team recognized that text-messaging was a contextually appropriate medium for a healthcare intervention in their setting. Supporting this assumption are national statistics that reveal that in Argentina from 2010 to 2013, the number of mobile phones in service had increased from 50.4 to 59.6 million and the number of SMS text messages increased from 5.8 to 11.3 billion per month.40 With an estimated population of 40.9 million,41 Argentina has more mobile phones in service than inhabitants.
Developing a strong patient-healthcare professional relationship through supervision and support has been identified as highly important in TB control efforts39,42,43 with the suggestion that improving relationships could potentially be achieved through telecommunication tools, such as texting.4 In the current study, in order to elicit the potential relationship benefit the team agreed that the intervention must include the interactive function of SMS, not be too automated, and not simply send reminders or information like reported in other studies.10,14,15,44 The intent for the intervention to not be ‘too automated’ was to establish a more personal relationship with the patients and be able to identify problems that could be dealt with. However, the tradeoff is increased workload and time needed to implement the intervention.
Directly observed therapy (DOT), where a trained healthcare worker or treatment supporter observes medication ingestion daily, has been the WHO recommended intervention to assure drug adherence.31 However, it continues to be challenging to apply for patients and healthcare services in many communities globally.45–47 In settings where self-administration is the standard treatment delivery, other options to supervise, provide support and promote patient-provider relationships are needed and TextTB is such an intervention.
Challenges and Benefits to Collaborative Intervention Development
The basic study premise was provided by the PI, but final drafting and decision making was left open for discussion and team agreement. Although the aim of this intervention development was to apply a collaborative approach, this resulted in an extended development period. First, participation in this process takes time away from team members’ other daily duties. Second, as an international collaboration it required correspondence by email and then an extended time on site by the PI to work directly with team members. The development phase did take longer than expected and delayed the initiation of patient recruitment, extending the onsite stay for the PI. Similarly, Owens et al.3 reported an extended development phase by involving service users in the design and development which resulted in an intervention distinct from and not considered during initial planning. Although this initial developmental phase was written into the proposal in our case, participatory intervention development can be problematic when funding agencies typically expect well-formulated and established proposals. On the other hand, engaging clinicians and patients in the design phase can minimize problems and delays during implementation.
Educational Content and Theoretical Considerations
In this study decision making for educational message content could have been more quickly made based on expert knowledge by the team alone. However, gaining insight from patients was essential and the added steps of applying a theory, and conducting a content analysis of patient-directed educational material provided the team with an extensive list of message options. In addition, the theory helped organize messages into categories, facilitate combining message types, and guide decisions. This process made message content development more systematic and comprehensive. The model was also applied in drafting the confirmation of receipt of medication administration text messages by including motivational messages.
The IMB model makes the assumption that individuals who are well-informed and motivated will develop behavior skills needed for effective adherence, but also takes into consideration contextual factors, such as living conditions and access to healthcare.19 Factors such as access to healthcare and stigma have been identified as a barrier to TB treatment adherence.48,49 An underlying premise for using text-messaging as the mode of intervention delivery was to mitigate the barrier that limited access to healthcare presented. The team recognized that many of their patients who attend this clinic come from throughout the region and could travel a few hours to arrive. We included a message acknowledging the stigma of TB in the general public. A number of patients responded and agreed with this message. Acknowledging challenges was a category coded under the contextual factor category and applied in a message combined with a behavior skill suggestion. The timing and ordering of message delivery was also considered. TextTB was designed to be applied at treatment initiation. When assessing SMS as a potential tool for patients living with HIV, Mbuagbaw and colleagues,50 identified initial treatment as a period when patients tended to be most forgetful.
Conclusion
This study supports the use of a collaborative approach and applying the IMB model to support message development. Interventions for TB care should be standardized, but also flexible and based on the needs of the local community. A collaborative approach involving local TB experts and patients during the design stage may have taken more time, but resulted in an intervention that was responsive to patient needs, culturally appropriate and comprehensive. The process required flexibility, an open mind and willingness to adapt to the needs and schedules of others. Applying the IMB model to systematically identify educational messages with adherence-related information, motivations and skill development and contextual language, along with expert knowledge and patient input, was useful in selecting the educational text content. Although health behavior theories can help guide the process of understanding underlying behavior change, more research is needed to test theory driven interventions to improve outcome for patients with TB. Additionally, text messaging as a mode to foster patient-provider relationship and provide a supportive mode of treatment delivery warrants further exploration.
Practice Implications
Regardless of the mode of delivery, collaboration among multidisciplinary research team members who would implement the intervention and patients who would potentially receive the intervention is important in development. Although potentially challenging during grant writing, planning for an extended time to collaborate with end users during design phase is necessary for successful implementation. Specific to SMS mode of delivery, issues that must be taken into consideration during development include timing of delivery, adapting to SMS format by using accepted and recognized abbreviations while considering cultural language nuances, and ordering of messages for optimum effect. Adaptation to SMS format will vary by country and language; therefore using local staff to develop messages is essential for content validity. Applying a theory to develop a coding scheme for content analysis of a body of educational literature can aid in systematic selection of content and provide structure and organization. SMS is a basic feature common in most phones and its use in TB management and other health interventions warrants consideration and systematic investigation.
Acknowledgements
We thank the patients and the hospital staff for their participation, special thanks to staff members Daniel Cardinale, Neli Peliza, Gabriela Laborde.
Authors Contributions
SI, SB, PP, and FR conceived and designed the study. SI, SB, CC, and ME were involved in intervention design. SI, SB, PP drafted the article. All authors contributed to review and revision, and approved the submitted version.
Funding
The study was funded through a Ruth L. Kirschstein National Research Service Award (NRSA) (grant no. F31NR012614), NINR and a research grant from Sigma Theta Tau International, Gamma Rho Chapter.
Disclosure
The corresponding author is the recipient of an NRSA and was a Fogarty International Clinical Research Scholar (2008–2009) during which time initial collaboration was established with members of the research team.
Declaration of Conflicting Interests
The authors declare that there is no conflict of interest.
References
1. Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev. 2010;32:56–69. ![]()
2. Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36: 165–73. ![]()
3. Owens C, Farrand P, Darvill R, Emmens T, Hewis E, Aitken P. Involving service users in intervention design: a participatory approach to developing a text-messaging intervention to reduce repetition of self-harm. Health Expect. 2010;14:285–95. ![]()
4. Barclay E. Text messages could hasten tuberculosis drug compliance. Lancet. 2009;373:15–6. ![]()
5. Mohammed S, Siddiqi O, Ali O, et al. User engagement with and attitudes towards an interactive SMS reminder system for patients with tuberculosis. J Telemed Telecare. 2012;18:404–8. ![]()
6. International Telecommunication Union. The World in 2013: ICT Facts and Figures. In: database WTII, (ed.). 2013.
7. Wu R, Appel L, Morra D, Lo V, Kitto S, Quan S. Short message service or disService: issues with text messaging in a complex medical environment. Int J Med Inform. 2014;83:278–84. ![]()
8. Gold J, Lim MS, Hellard ME, Hocking JS, Keogh L. What’s in a message? Delivering sexual health promotion to young people in Australia via text messaging. BMC Public Health. 2010;10:792. ![]()
9. Bridges.org. Executive summary: Testing the use of SMS reminders in the treatment of Tuberculosis in Cape Town, South Africa. 2005.
10. Chen ZW, Fang LZ, Chen LY, Dai HL. Comparison of an SMS text messaging and phone reminder to improve attendance at a health promotion center: A randomized controlled trial. J Zhejiang Univ Sci B. 2008;9:34–8. ![]()
11. Coomes CM, Lewis MA, Uhrig JD, Furberg RD, Harris JL, Bann CM. Beyond reminders: a conceptual framework for using short message service to promote prevention and improve healthcare quality and clinical outcomes for people living with HIV. AIDS Care. 2011;24:348–57. ![]()
12. De Costa A, Shet A, Kumarasamy N, et al. Design of a randomized trial to evaluate the influence of mobile phone reminders on adherence to first line antiretroviral treatment in South India – the HIVIND study protocol. BMC Med Res Methodol. 2010;10:25. ![]()
13. Kunawararak P, Pongpanich S, Chantawong S, et al. Tuberculosis treatment with mobile-phone medication reminders in northern Thailand. Southeast Asian J Trop Med Public Health. 2011;42:1444–51.
14. Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25:825–34. ![]()
15. Vervloet M, van Dijk L, Santen-Reestman J, et al. SMS reminders improve adherence to oral medication in type 2 diabetes patients who are real time electronically monitored. Int J Med Inform. 2012;81: 594–604. ![]()
16. Furberg RD, Uhrig JD, Bann CM, et al. Technical Implementation of a Multi-Component, Text Message-Based Intervention for Persons Living with HIV. JMIR Res Protoc. 2012;1:e17. ![]()
17. World Health Organization. TB country profile Argentina, 2012. 2014.
18. Instituto Nacional de Enfermidades Respiratorias E. Coni. [RESULTADO DEL TRATAMIENTO DE LOS CASOS DE TUBERCULOSIS. Situación nacional y por jurisdicción, República Argentina, 1980–2008]. 2010.
19. Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25:462–73. ![]()
20. Munro S, Lewin S, Swart T, Volmink J. A review of health behaviour theories: how useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS? BMC Public Health. 2007;7:104. ![]()
21. Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–74. ![]()
22. Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002;21:177– 86. ![]()
23. Kanjee Z, Amico KR, Li F, Mbolekwa K, Moll AP, Friedland GH. Tuberculosis infection control in a high drug-resistance setting in rural South Africa: information, motivation, and behavioral skills. J Infect Public Health. 2012;5:67–81. ![]()
24. Franks J CP, Hirsch-Moverman Y & Charles P. Adherence to Treatment for Latent Tuberculosis Infection: A Manual for Health Care Providers. New York, NY 2005, p.1–59.
25. Iribarren S, Beck S, Pearce PF, et al. TextTB: A mixed method pilot study evaluating acceptance, feasibility and exploring initial efficacy of a text messaging intervention to support TB treatment adherence. Tuberculosis Research and Treatment 2013; Volume 2013, Article ID 349394: 12 pages.
26. Denzin NK and Lincoln YS. Handbook of qualitative research. Thousand Oaks: Sage, 2000.
27. Krippendorff K. Content Analysis: An Introduction to its Methodology. Thousand Oaks, CA: Sage, 2004.
28. Neuendorf KA. The content analysis guidebook. Thousand Oaks, CA: Sage, 2002.
29. Chirico C, Kuriger A, Etchevarria M, Casamajor L, Morcillo N. [Anti- tuberculosis treatment evaluation in northern districts of Buenos Aires suburbs]. Medicina (B Aires). 2007;67:131–5.
30. Caminero JA. Guía de la tuberculosis para médicos especialistas. Saint Michel, Paris – Francia: Union Internacional Contra la Tuberculosis y Enfermedades Respiratorias (UICTER) 2003.
31. World Health Organization. Treatment for Tuberculosis: Guidelines (4rd Edition) WHO/HTM/TB/ 2009.420. 3rd ed. 2009.
32. Lim MS, Hocking JS, Hellard ME, Aitken CK. SMS STI: a review of the uses of mobile phone text messaging in sexual health. Int J STD AIDS. 2008;19:287–90. ![]()
33. Person AK, Blain ML, Jiang H, Rasmussen PW, Stout JE. Text messaging for enhancement of testing and treatment for tuberculosis, human immunodeficiency virus, and syphilis: A survey of attitudes toward cellular phones and healthcare. Telemed J E Health. 2011;17:189–95. ![]()
34. DeMaio J, Schwartz L, Cooley P, Tice A. The application of telemedicine technology to a directly observed therapy program for tuberculosis: A pilot project. Clin Infect Dis. 2001;33:2082–4. ![]()
35. Hoffman JA, Cunningham JR, Suleh AJ, et al. Mobile direct observation treatment for tuberculosis patients: A technical feasibility pilot using mobile phones in Nairobi, Kenya. Am J Prev Med. 2010;39: 78–80. ![]()
36. Wade VA, Karnon J, Eliott JA, Hiller JE. Home videophones improve direct observation in tuberculosis treatment: A mixed methods evaluation. PLoS One. 2012;7:e50155. ![]()
37. Lester RT, Ritvo P, Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): A randomised trial. Lancet. 2010;376:1838–45. ![]()
38. Mbuagbaw L, Thabane L, Ongolo-Zogo P, et al. The Cameroon mobile phone SMS (CAMPS) trial: a protocol for a randomized controlled trial of mobile phone text messaging versus usual care for improving adherence to highly active anti-retroviral therapy. Trials. 2011;12:5. ![]()
39. World Health Organization. The Global Plan to Stop TB 2011–2015. Transforming the fight towards elimination of tuberculosis. 2009.
40. Instituto Nacional de Estadistica y censos (INDEC). Servicios Publicos. Argentina 2013.
41. Instituto Nacional de Estadistica y censos (INDEC). Censo Nacional de Población Hogares y Viviendas [National household censis]. Argentina 2001.
42. Iribarren S, Rubinstein F, Discacciati V and Pearce PF. Barriers and facilitators to successful treatment of tuberculosis in a high TB burden region in Argentina [in progress]. 2011.
43. World Health Organization. The Stop TB Strategy. Building on and enhancing the DOTS to meet the TB-related millennium development goals. 2006.
44. Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther. 2009;11:99–106. ![]()
45. Hill PC, Stevens W, Hill S, et al. Risk factors for defaulting from tuberculosis treatment: A prospective cohort study of 301 cases in the Gambia. Int J Tuberc Lung Dis. 2005;9:1349–54.
46. Khan MA, Walley JD, Witter SN, Imran A, Safdar N. Costs and cost-effectiveness of different DOT strategies for the treatment of tuberculosis in Pakistan. Directly Observed Treatment. Health Policy Plan. 2002;17:178–86. ![]()
47. Sanchez AI, Bertolozzi MR. Beyond DOTS (Directly Observed Treatment Short-Course) in tuberculosis’ control: Interfacing and sharing needs. Rev Lat Am Enfermagem. 2009;17:689–94. ![]()
48. Cramm JM, Finkenflugel HJ, Moller V, Nieboer AP. TB treatment initiation and adherence in a South African community influenced more by perceptions than by knowledge of tuberculosis. BMC Public Health. 2010;10:72. ![]()
49. Enarson DA and Billo NE. Critical evaluation of the Global DOTS Expansion Plan. Bull World Health Organ. 2007;85:395–8; discussion 9-403.
50. Mbuagbaw L, Bonono-Momnougui RC, Thabane L. Considerations in using text messages to improve adherence to highly active antiretroviral therapy: A qualitative study among clients in Yaounde, Cameroon. HIV AIDS (Auckl). 2012;4:45–50.
51. Bediang G, Stoll B, Elia N, et al. SMS reminders to improve the tuberculosis cure rate in developing countries (TB-SMS Cameroon): a protocol of a randomised control study. Trials. 2014;15:35. ![]()
52. Nglazi MD, Bekker LG, Wood R, Hussey GD, Wiysonge CS. Mobile phone text messaging for promoting adherence to anti-tuberculosis treatment: a systematic review. BMC Infect Dis. 2013;13:566. ![]()

