A Qualitative Study Exploring Stakeholder Perceptions of Video Directly Observed Therapy for Monitoring Tuberculosis Treatment in the US-Mexico Border Region
María Luisa Zúñiga, PhD1, Kelly Collins, PhD2, Fátima Muñoz, MD, MPH2, Kathleen Moser, MD, MPH3, Gudelia Rangel, PhD4, Jazmine Cuevas-Mota, MPH2, Maureen Clark, BA2, Jose Luis Burgos, MD, MPH2, Richard S. Garfein, PhD, MPH2
1San Diego State University, School of Social Work, 5500 Campanile Drive, San Diego, CA, USA; 2Division of Global Public Health, Department of Medicine, University of California, San Diego, La Jolla, CA, USA; 3San Diego County Health and Human Services Agency, San Diego, CA, USA; 4Comisión de Salud Fronteriza, Sección México-Secretaria de Salud, Tijuana, Baja California, México
Corresponding Author: mlzuniga@mail.sdsu.edu
Journal MTM 5:2:12–23, 2016
Background: Tuberculosis (TB) incidence in the U.S.-Mexico border region exceeds both countries’ national rates. The four U.S. states bordering Mexico account for nearly 40% of total U.S. TB cases. TB treatment monitoring using directly observed therapy (DOT) is a globally-accepted practice; however, it is resource intensive for providers and patients.
Aims: To determine whether Video DOT (VDOT)—a process whereby patients record themselves taking their medication by mobile phone and sending the videos to their TB care provider for observation—could be used to remotely monitor TB treatment adherence.
Methods: We conducted five focus groups with TB patients and four with TB care providers in San Diego, California, U.S. and Tijuana, B.C., Mexico.
Results: VDOT consistently received broad support: U.S. patients valued greater autonomy and Mexican patients valued improved privacy. Groups agreed technology would not be a barrier, but emphasized need for adequate patient training.
Conclusion: Patients and providers in both countries found VDOT conceptually feasible and acceptable.
Introduction
Tuberculosis (TB) now surpasses HIV as the leading cause death from an infectious disease and is also the number one killer of HIV-infected persons.1–3 TB occurs in both developing and developed countries and remains a persistent problem among populations living in the United States (U.S.)-Mexico border region.4,5 In 2012, there were 9,951 new reported cases of TB in the U.S. (3.2/100,000 population).6 However, the U.S. border states—California, Arizona, New Mexico, and Texas—account for almost 3,700 TB cases (~40% of total U.S. cases), with incidence rates of 5.8, 3.2, 1.9 and 4.7 per 100,000 pop., respectively.7 TB incidence in Mexico’s northern border states is also substantially higher than Mexico’s overall incidence (16.8/100,000 pop.), with Baja California (California’s sister state) bearing the greatest burden in all of Mexico (58.5/100,000 pop.).8
While TB can be effectively treated with antibiotics, treatment typically takes 6 months and may extend to 24 months for patients with drug resistant TB. Moreover, adherence to medication regimens is critical to avoid prolonged periods of infectiousness, relapse, and the emergence of drug resistant strains. The U.S. Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO) and Mexico’s National Center for Preventive Programs and Disease Control (CENAPRECE) all recommend Directly Observed Therapy (DOT) as an essential component of patient care for TB in order to ensure adherence and stem TB transmission and drug resistance.8,9 DOT is a patient-centered approach to treatment in which patients are observed ingesting each dose of anti-TB medication and is intended to maximize the likelihood that patients will complete therapy.10 It can be provided in the patient’s home, a clinic, or other mutually agreed upon location.
In Mexico, as in the U.S., local health jurisdictions dictate the allocation of resources for DOT. Since cities such as Tijuana have limited resources for TB services, DOT is not possible for all TB patients.11 Although, studies have shown that DOT is highly effective in achieving high TB treatment adherence, especially when combined with individualized care;12,13 DOT can limit patient mobility and privacy, involves travel costs and may be especially difficult for patients who live far from health clinics. Traditional DOT is poorly suited for patients who are highly mobile or have limited availability during traditional clinic hours (e.g., work or school), or travel out of the country, which happens frequently in U.S.-Mexico border cities. DOT modalities that are responsive to the needs of these patients are needed to improve adherence and completion of TB treatment, especially among patients who may require binational care coordination, as offered through the San Diego County CURE TB Referral Program.14
Use of mobile health (mHealth) technology to improve patient care continuity, including DOT, has captured the interest and imagination of researchers and clinicians who envision how technology can promote medication adherence through improved self-care practices.15 Prior work applying technologyto ease the time- and resource-intensive demands of traditional DOT includes using landline phones with video monitors to allow health department staff to remotely observe patients taking their medications.16,17 Little data are available on this form of “Video DOT” (VDOT), because this approach has been used only in small pilot studies or adopted by TB programs without a research component. Studies evaluating VDOT using mobile phones, instead of landline phone, are currently underway, but few have been published to date. These include a feasibility study in Kenya,18 and work completed by members of our own team to pilot test VDOT involving videos recorded by TB patients using smartphones, which are subsequently observed by a healthcare provider through a secure website.19 Interventions that make use of video capabilities available on most cell phones, however, have been largely unexplored for TB medication adherence and pose a promising application for TB patients in both low- and high-resource settings.20
The current binational qualitative study was undertaken to assess the acceptability and feasibility of cell phone-based VDOT for monitoring TB treatment adherence in the U.S.-Mexico border region prior to developing and pilot-testing the application. This paper presents the results of a qualitative study conducted to inform the design and implementation of a subsequent binational pilot study of a VDOT application for TB treatment monitoring.19
Methods
Study Population
This qualitative study was conducted collaboratively by the University of California San Diego and the TB control programs of San Diego County and Tijuana. In San Diego, care for active TB cases is centralized through the county’s Tuberculosis Control Program. In Tijuana, TB control is overseen by the Secretary of Health of Baja California at the state level and is managed by the local sanitary jurisdiction in conjunction with care delivery through local health centers.21
Recruitment and enrollment
A convenience sample of TB patients, care providers (e.g., physicians, nurses and DOT workers) and local TB public health officials were invited to participate in focus groups. TB patients who had completed treatment within the past six months or were still on treatment but non-infectious, and had received traditional in-person DOT (hereafter referred to as “patients”) were invited by TB control program staff in each city to participate. Patient eligibility criteria included: age ≥ 18, completed at least three months of TB treatment and tested smear or culture negative for M. tuberculosis, and able to speak English or Spanish. TB providers (nurses and physicians) and DOT workers on both sides were invited to participate in the focus groups through their respective TB control programs. Eligibility criteria included: age ≥ 18 years, able to speak English or Spanish, and currently providing TB clinical care, DOT, case management or outreach to TB patients.
Focus groups were conducted in the participants’ native language (English/Spanish) by facilitators who were members of our study research team (MZ, KC, JCM, JLB and RSG). Written informed consent including permission to tape-record the sessions for transcription and coding purposes was obtained from all participants. Participants completed a brief demographic questionnaire. San Diego patient participants were offered a gift card worth $20.00 USD and Mexican participants were offered a comparable amount of $200 Mexican pesos as remuneration for their time and travel.
Ethics Statement
The study was approved by the Institutional Review Board at the University of California, San Diego and the Bioethics Committee of El Colegio de la Frontera Norte (COLEF) in Tijuana.
Focus group procedures
Separate focus groups were held for patients and providers. The facilitator briefly described VDOT as a method of monitoring medication intake by using a smartphone to capture a video of someone (patient) taking their TB medication and then automatically sending the video in an encrypted manner to their care provider for observation (Figure 1). Facilitators informed the participants that videos could not be viewed on the cell phone and only health department personnel would have access to the videos. Each focus group started with a facilitator reading aloud the study purpose and voluntary nature of participation. Following the introduction, the facilitator used a semi-structured focus group interview guide (see Appendix 1 patient guide, Appendix 2 provider guide) to elicit participant reactions to VDOT and obtain participant perceptions of the overall feasibility and acceptability of VDOT, as well as advantages/disadvantages of VDOT versus traditional in-person DOT. Participants were also asked to identify patient characteristics that could make VDOT better suited for some patients than others, and to provide recommendations for overcoming possible technological barriers to using VDOT.
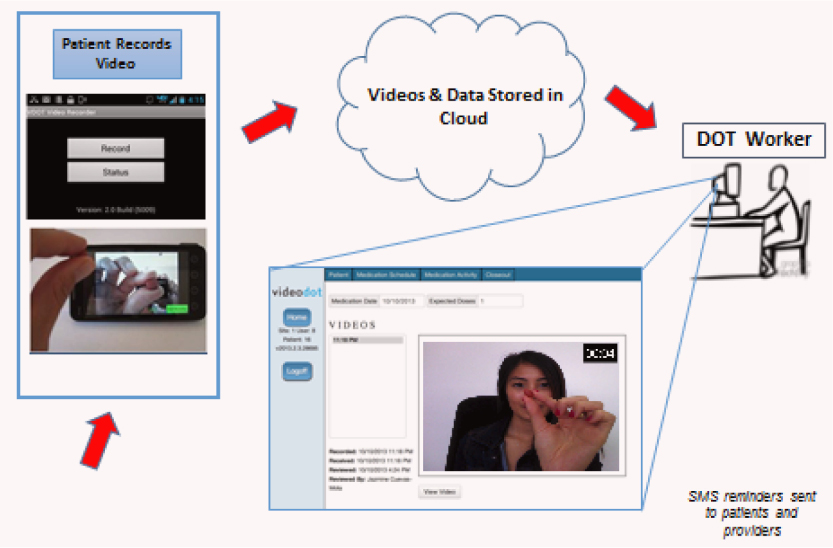
Figure 1: Informing a binational video cell phone directly observed therapy trial for Tuberculosis.17
Provider focus group questions elicited feedback on intervention procedures, preferred patient characteristics and possible enhancements to maximize adherence or lower cost. Participants were also asked to comment on the potential barriers and facilitators of using smartphones to record and send videos of patients ingesting their medications.
Analysis of Qualitative Data
Constant Comparative Analysis Methods—a structured data coding process that allows for jointly coding data to explore the breadth of responses within primary themes—were used to analyze the focus group transcripts.22–24 We applied theoretical thematic analysis procedures based on Braun and Clarke’s work25 to identify patterns within our focus group data based on our interest to understand participant perspectives on the proposed VDOT intervention. Our a priori themes for this qualitative study followed recommendations for conducting feasibility studies described by Bowen and colleagues,26 particularly when there was a lack of prior studies on a specific intervention among a population of interest that may have distinct needs or interests. Drawing on Bowen and colleagues’ work, we applied the following general focus areas to guide our exploratory work and understand the feasibility of VDOT in a binational context: Acceptability (reaction to the proposed intervention), Demand (estimated use of the intervention) and Practicality (evidence of potential efficacy amidst individual, time, commitment or other constraints). Our major a priori themes were: 1) perceived intervention feasibility and acceptability; 2) technical recommendations; 3) patient-provider relationship and interactions; and 4) characteristics of good VDOT candidates.
Focus group data were audio-recorded and discussions were summarized. Spanish-language focus group summaries were translated into English by a bilingual/bicultural study team member (JCM). Two study team members (MLZ and KC) developed initial categories and a coding scheme based on the a priori themes and conducted a detailed review of patient focus group summaries (i.e., open coding). The two study team members independently reviewed and coded the transcripts by hand using the coding scheme. The coders then met to discuss and refine categories, resolve coding discrepancies, refine coding interpretation and assign new codes as needed. Final coded transcripts included patient and provider recommendations and concerns surrounding implementation and perceived feasibility and acceptability of VDOT. The analytic process considered potential differences and similarities between patient and provider perspectives, as well as indicators of cross-cultural or binational differences between them. Demographic data were described using SPSS 16.0.
Results
Participant Characteristics
In total, nine focus groups were conducted—six in San Diego (four with patients; two with DOT workers and providers together) and three in Tijuana (one each with patients, providers and DOT workers separately). Overall, 22 patients and 47 staff took part in the groups. Sessions ranged from 46 to 103 minutes (mean=82 minutes). San Diego’s 14 patient respondents were ethnically diverse, including 8 Latinos (57%). Racial background (including Latinos) was as follows: 4 (29%) Asian, 2 (14%) Caucasian/White, 2 (14%) African American, 3 (21%) other, and 3 (21%) who preferred not to respond. Detailed demographic information provided in (Table 1) show that study participants were diverse in terms of age, gender, race/ethnicity and socio-economic status. Patients spent an average of 7.4 months having their treatment monitored through in-person DOT in San Diego and average of 8 months in Tijuana. Owning a cell phone was reported by 8 (57%) patients in San Diego and 7 (88%) patients in Tijuana. Overall, 9 patients (41%) (5 [37.5%] in San Diego and 4 [50%] in Tijuana) reported prior experience sending a picture from their cell phone and 4 patients (2 [14.3%] in San Diego and 2 [25%] in Tijuana) reported prior experience sending a video from a cell phone.
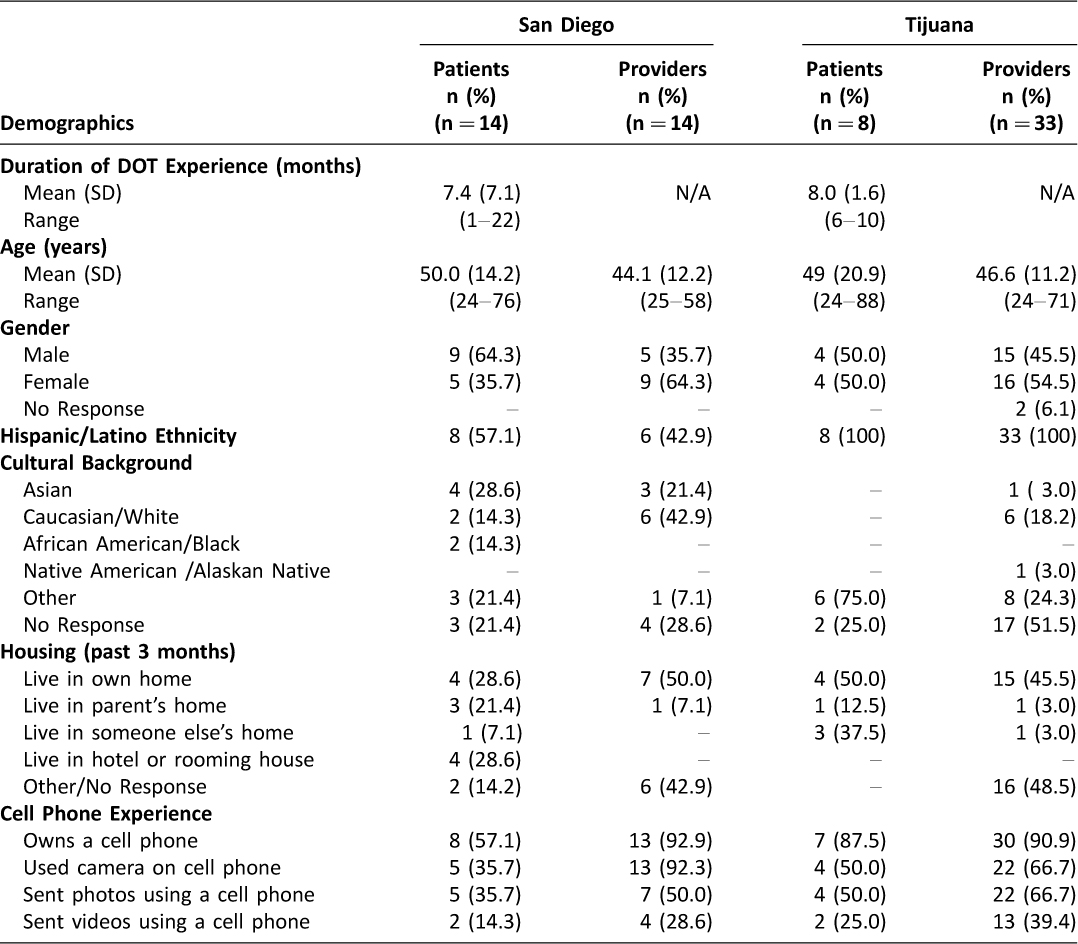
Table 1: Participant demographic and technology experience profile by study site
Theme 1: Perceived implementation feasibility and acceptability of VDOT
Both patients and providers felt that VDOT was a feasible and acceptable alternative to in-person DOT. Overwhelmingly, patients from Tijuana and San Diego stated that VDOT could be a convenient way to receive DOT for TB treatment. They felt that it would make their lives easier and that VDOT would improve patient acceptability of DOT in general, as one patient described:
“With the demonstration that has been shown, I think it’s really easy to use.” (Female patient, San Diego)
A DOT worker noted:
“For us as promotores the benefit here [Tijuana] would be for the patients, especially during these times of rain we don’t have access to them and it would also benefit those who live far. I believe that those are the benefits for us.” (Male DOT worker, Tijuana)
San Diego patients reported that VDOT could provide a sense of independence, trustworthiness, freedom of mobility and convenience (e.g., not needing to wait at home for the DOT worker to arrive). They also mentioned that with in-person DOT they sometimes felt patronized and untrusted:
“… I feel like I was being babysat, I’m an adult …” (Male patient, San Diego) and
“It’s upsetting in the initial stages. I was upset because, like these people don’t trust me. I am an adult. I am responsible. I want to be cured.” (Female patient, San Diego).
The notion of in-person DOT as paternalistic was not evident among Tijuana patients who focused more on VDOT allowing greater flexibility of daily mobility. Patients in both cities felt that VDOT could help alleviate privacy concerns associated with DOT because a clinician or DOT worker would not be required to routinely visit the patient’s home or work place. Clinic staff from Tijuana felt that VDOT had the potential to save time and money for their patients:
“It’s a bit of work that we will have to do with this program, but I see it as 10 fewer trips during the day …. It will avoid having to go out in the unit/vehicle.” (Male DOT worker, Tijuana)
It also reduced the burden on patients who received clinic-based DOT as noted by this patient:
“As a TB patient, it would be great not having to show up at the clinic every day.” (Female patient, Tijuana)
Theme 2: Technical support and recommendations
Sufficient patient training and technical support to use VDOT were the major concerns in all groups. Patients in both cities expressed concern that the technology might be hard for some individuals to learn and use, but also stated that adequate preparation and training could help to overcome potential problems. Patients and providers offered specific technical recommendations to facilitate successful uptake of VDOT. San Diego patients focused on the need for understanding their TB disease first before attempting to initiate VDOT. Tijuana patients expressed concern about cellular coverage while traveling outside the region and whether the proposed VDOT program included sufficient training on how to perform the procedures. As one participant mentioned:
“I do not know how to operate this type of device, but if I get a good phone and someone to tell me everything on [how] to use it, I can do it.” (Female patient, Tijuana)
Providers in both cities also emphasized the need for sufficient patient and staff training and ongoing technical support. San Diego providers focused on adequacy of the VDOT training protocol, how to tailor VDOT to the needs of patients (e.g., Spanish-language dominant patients), maintaining patient confidentiality (e.g., during recording and after transmission of videos), and liability of sending video information. Tijuana clinic staff were more focused on number of hours of patient and staff training. As one provider noted:
“… we also have to consider how confident the patient is handling a camera. Many of them are illiterate; many of them are patients who don’t have greater resources other than their family who tells them how to do things or does them for them.” (Male provider, Tijuana)
Theme 3: Patient-provider relationship and interactions
A theme across focus groups in both cities was concern over how the patient-provider relationship might change with VDOT. Patients in both cities indicated some concern over losing contact with the DOT worker, as one participant noted:
“You would lose that personal touch … the worker comes to you, smiling and says, ‘hey, how are you?’ and everything. It helps boost your ego right, because somebody cares for you.” (Female patient, San Diego)
A second participant alluded to the expanded role of the promotor in supporting individual patient’s health:
“My promotor helped me out a lot. She would bring me the cup for my bacilloscopy [sputum smear], she would remind me of certain things, an important date, etc. Truthfully, it really is necessary for the promotor to come to our homes.” (Male patient, Tijuana)
San Diego patients felt that this would be less problematic if prior interaction with the DOT worker included instruction on how to use VDOT, and educating the patient to help them become less reliant on the DOT worker and more confident on how to use VDOT. The reduction in patient-provider contact was noted, but it was less important among San Diego patients who placed greater value on the opportunity to gain independence.
San Diego providers mentioned concerns over potential loss of face-to-face communication with patients, but this was not as prominent as technical and training concerns. Not surprisingly, loss of interpersonal communication or interaction was expressed most strongly among Tijuana DOT workers. They felt that the trust and personal relationship with patients could be jeopardized by VDOT, because the time they spent with patients was important for building trust.
“There is something to be said about having that face-to-face interaction at the beginning … So, that’s where things like reliability and you know, being able to trust them to begin with, that they are actually going to [take their medication] in a way that is going to benefit them in the long run is concerning to us …” (Female provider, San Diego)
Another provider commented:
“When we go and give them their medication and watch them take it, it’s not just watching them and thinking they already took and it I’m leaving … We stay with them, talk to them, ask how things are going, how they’re feeling, etc. That’s how we gain their trust and we appreciate that. Hence, that would be lost.” (Female provider from Tijuana)
During the course of the focus group discussion, Tijuana DOT workers identified a positive potential impact of VDOT on the patient-provider relationship. They considered that VDOT may free up some of their time with patients who are doing well and allow them to focus efforts and time with those patients who need closer follow-up and more direct contact.
Theme 4: Characteristics of “good candidates” for VDOT
Patients and providers in both cities offered recommendations about the profiles of patients who would and would not be good candidates for VDOT. For example, patients recommended that individuals who lacked familiarity with technology might be poor candidates, citing older patients as an example. Patients felt that some older patients might lack experience or comfort needed to use technology to record their treatment and would be unsuccessful and/or non-adherent to their medication if they were enrolled in VDOT. Patients felt that to participate, VDOT candidates needed to be willing to adhere to VDOT protocols. Tijuana patients specifically mentioned that persons who inject drugs and/or who are homeless may not be good VDOT candidates because their lifestyle could adversely affect their willingness or ability to be adherent. Tijuana patients and clinic staff commented about how some may try to make it look like they swallowed the pills but had not.
Providers in both cities felt that individuals with complicated disease such as multi-drug resistant TB or co-morbid conditions (e.g., HIV or diabetes) may also not be good candidates for VDOT. Tijuana providers were more specific about their perceptions of which patient circumstances would make them less desirable candidates for VDOT, including patients who were hospitalized, in drug abuse treatment, or undergoing other treatments.
Patients in both cities also indicated that certain patients may be more likely to lose, break, or sell the mobile phone loaned to them for VDOT. They reported that patients whose environments pose increased risk for phone theft might be poor candidates. Participants recommended contingencies for these cases, including mandated penalties for losing the VDOT phone and signing contractual agreements for patients to cover the cost of lost/stolen/broken cell phones. Participants explained:
“I think that if a patient will put a deposit until it’s finished, then they will take care of it …” (Female patient, San Diego)
“Maybe a written agreement, with terms and conditions [would help to get the phones back] …” (Female patient, San Diego)
Discussion
To our knowledge, this is the first study to qualitatively assess patient and provider perspectives about the use of mHealth interventions for TB treatment adherence monitoring, as well as the first to be conducted in a binational setting. This study explored patient and provider perceptions on a novel VDOT intervention to monitor and improve adherence to TB treatment. We found that overall, patients and providers on both sides of the border believed that the proposed intervention was feasible and acceptable, especially if the research team addressed specific areas of concern and considered participant recommendations. Participants also provided concrete and useful advisement that informed a subsequent VDOT pilot study.19
Patient and provider insights into VDOT feasibility and acceptability indicated that VDOT could play an important role in supplementing the array of TB care continuity approaches currently used in San Diego and Tijuana. Patient acceptability was demonstrated by interest in how VDOT could promote medication adherence autonomy and patient privacy. Providers saw VDOT as an additional tool for assuring TB treatment adherence. Patient literacy and comfort with technology, adequate training and technical support were among the recommendations for implementing VDOT.
An important finding was that patients and clinic staff from San Diego and Tijuana shared some priorities and perspectives on VDOT, while differing on others. Subtleties in patient and provider focus group discussions indicate that commonalities in perspectives may have different underlying reasons. For example, San Diego patient concerns about adequate training were in the context of having sufficient self-efficacy to use VDOT independently. Conversely, San Diego provider concerns about adequate patient training were more related to ensuring that clinicians could rely on VDOT to effectively monitor patient adherence. This difference in perspectives is not new, as members of our research team have documented in earlier studies that physician and patient agreement on specific barriers to health care, may in fact be due to vastly different underlying reasons.23 For example, in a study conducted by Zúñiga and colleagues on barriers to HIV clinical trials participation in San Diego, patients and providers agreed that lack of transportation to the clinic was a barrier.23 Qualitative study findings revealed, however, that Latino participants were apprehensive about taking public transportation due to immigration concerns, while providers perceived it as a lack of transportation.27
Cultural differences between San Diego and Tijuana patients were revealed in perspectives about the patient-provider relationship. Tijuana patients expressed concern that VDOT might jeopardize face-to-face contact with their providers. This was also a concern mentioned by San Diego patients; however, patient independence in managing their treatment was of greater relative importance.
In comparison to the U.S. health care system, the Mexican health care system generally has a more paternalistic approach to care delivery where patients are expected to comply unquestioningly with medical directives. We saw this reflected in Tijuana patient expectations for receiving sufficient training and support, and when referring to consequences when they do not adhere to the VDOT protocol. Members of our study team (FM, MLZ) have identified similar patient perspectives where patients living with HIV felt scolded by providers when they were unable to adhere to medication.28 San Diego patients were oriented more towards how VDOT could promote greater independence in health care management. These findings underscore the need for clinicians and researchers to understand and manage expectations of patient self-reliance to participate in VDOT.
Limitations and feasibility issues of implementing the VDOT intervention merit attention. Since the purpose of this study was to inform the development of a VDOT application that was previously non-existent, costs related to the mobile devices, cellular service, and program implementation were not assessed. Costs, as well as actual feasibility and acceptability of the resulting VDOT system were assessed in a subsequent pilot study conducted in San Diego and Tijuana.19
Other limitations inherent to small qualitative studies are that we relied on a convenience sample of participants who may not represent other TB patient or provider perspectives in other communities. Since patient eligibility criteria limited the number of potential participants, and clinic staff participation was limited by availability, study findings might not be representative of all TB patients and providers. However, obtaining patient and provider perspectives in high- and low-resource communities allowed for enhanced sensitivity to city-specific opinions and expectations to inform the development and subsequent evaluation of the VDOT system. In addition, the broad-scale, binational engagement of health departments provides critical information about how patients and providers perceive TB treatment monitoring and how it affects their lives, not as patients but as individuals. Finally, the opinions of the focus group participants were based on a hypothetical example of how VDOT would be used; however, it is unknown how these opinions would differ if the patients were shown a working example of VDOT or were given an opportunity to use it.
Conclusion
Results of this study indicate that TB patients and providers in San Diego and Tijuana considered VDOT to be feasible and acceptable for monitoring patients ingesting their TB medications. Participants generally thought this approach would make adherence monitoring less burdensome and more confidential than in-person DOT. Detailed patient technical training and ongoing support for both patients and providers appeared to be essential for successful implementation of a VDOT program. Findings from this study underscore important considerations about differences in the culture of health care delivery context (U.S. versus Mexico). Country-specific considerations regarding patient and provider expectations about the patient role in their care, patient health outcomes, and patient satisfaction with care are especially important given the great potential for mHealth interventions to be applied transnationally.
Our work highlights the role that the culture of health care delivery can play in perceived risks and benefits of VDOT and future mHealth applications. Importantly, the binational nature of this study allowed us to identify overt and nuanced differences and similarities in concerns and preferences of TB patients and providers around the use of mHealth globally. Study findings were used to inform the subsequent development and implementation of VDOT pilot study for TB treatment monitoring17. This study contributes much needed empirical data to guide mHealth innovation for addressing TB, as well as other diseases regions where scarce health care and manpower resources must be more strategically managed.
Acknowledgements
The authors wish to thank Deborah McIntosh, Gabriela Escalante, Cristhian Colin, Dr. José Guadalupe Bustamante, and Dr. Rafael Laniado-Laborín. For their efforts and for sharing insights that were crucial for developing the VDOT System. The authors also thank the study participants for the feedback they provided to help develop the system.
This study was funded by grants from the National Institutes of Health (R21-AI088326). JLB was also supported by NIMH grant K01-MH095680. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
1. World Health Organization (WHO). Global Tuberculosis Report 2015. 2015 [cited 2015 Dec 18]. Available from: http://www.who.int/tb/publications/global_report/en/
2. WHO. Global Update on HIV Treatment 2013: Results, Impact and Opportunities. 2013 [cited 2015 Dec 18]. Available from: http://apps.who.int/iris/bitstream/10665/85326/1/9789241505734_eng.pdf?ua=1
3. Roman J. Tuberculosis Surpasses HIV/AIDS As Leading Cause Of Global Death: WHO. 2015 [cited 2015 Dec 18]. Available from: http://www.techtimes.com/articles/100819/20151029/tuberculosis-surpasses-hiv-aids-as-leading-cause-of-global-death-who.htm
4. Baker BJ, Moonan PK. Characterizing tuberculosis genotype clusters along the United States-Mexico border. Int J Tuberc Lung Dis 2014;18(3):289–91. ![]()
5. The Pan American Health Organization [Internet]. TB in the US-Mexico Border Region. Winning the fight against TB: combining efforts of the research and civil society community. 2014 [cited 2015 Dec 18]. Available from: http://www.paho.org/hq/index.php?option=com_content&view=article&id=2511&Itemid=40275&lang=en
6. Morbidity and Mortality Weekly Report (MMWR). Trends in Tuberculosis —United States. The Centers for Disease Control and Prevention. 2013 [cited 2015 Dec 18]. Available from: http://www.cdc.gov/mmwr/pdf/wk/mm6211.pdf
7. United States Department of Health and Human Services. 2012 [cited 2014 Nov 26]. Available from: http://www.cdc.gov/tb/statistics/reports/2012/pdf/report2012.pdf
8. Secretaría de Salud de México. Misión de Evaluación Externa del Programa de Control de Tuberculosis. 2013 [cited 2014 Apr 9]. Available from: http://www.cenaprece.salud.gob.mx/programas/interior/micobacteriosis/descargas/pdf/reporte_final_mexico.pdf. 2013
9. MMWR. Treatment of Tuberculosis. 2003 [cited 2015 Apr 13]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5211a1.htm#top. 2003
10. WHO. The Stop TB Strategy. 2006 [cited 2015 Dec 18]. Available from: http://whqlibdoc.who.int/hq/2006/WHO_HTM_STB_2006.368_eng.pdf
11. Tuberculosis in the San Diego-Tijuana Border Region: Time for Bi-National Community-Based Solutions. International Community Foundation. 2010 [cited 2015 Dec 18]. Available from: http://www.icfdn.org/publications/TBReport/TB_REPORT_ENG_FINAL.pdf.
12. Radilla-Chávez P, Laniado-Laborín R. Results of directly observed treatment for tuberculosis in Ensenada, Mexico: not all DOTS programs are created equally. Int J Tuberc Lung Dis 2007;11(3):289–92. ![]()
13. Anuwatnonthakate A, Limsomboon P, Nateniyom S, et al. Directly observed therapy and improved tuberculosis treatment outcomes in Thailand. PLoS One 2008;3(8):e3089. ![]()
14. Cure TB Referral Program. San Diego County Health & Human Services Agency. 2015 [cited 2015 Apr 9]. Available from: http://www.sandiegocounty.gov/hhsa/programs/phs/cure_tb/
15. WHO mHealth: New Horizons for Health through Mobile Technologies, Global Observatory for eHealth Series – Volume 3. 2011 [cited 2015 Feb 13]. Available from: http://whqlibdoc.who.int/publications/2011/9789241564250_eng.pdf?ua=1
16. Hoffman JA, Cunningham JR, Suleh AJ, et al. Mobile direct observation treatment for tuberculosis patients: a technical feasibility pilot using mobile phones in Nairobi, Kenya. Am J Prev Med 2010;39(1):78–80. ![]()
17. Garfein R, Collins K, Munoz F, et al. High Tuberculosis Treatment Adherence Obtained Using Mobile Phones for Video Directly Observed Therapy: Results of a Binational Pilot Study. J Mob Technol Med 2012;1(4S):30. ![]()
18. Hoffman JA, Cunningham JR, Suleh AJ, et al. Mobile direct observation treatment for tuberculosis patients: a technical feasibility pilot using mobile phones in Nairobi, Kenya. Am J Prev Med 2010;39(1):78–80. ![]()
19. Garfein RS, Collins K, Muñoz F, et al. Feasibility of tuberculosis treatment monitoring by video directly observed therapy: a binational pilot study. Int J Tuberc Lung Dis 2015;19(9):1057–64. ![]()
20. Denkinger CM, Grenier J, Stratis AK, et al. Mobile health to improve tuberculosis care and control: a call worth making. Int J Tuberc Lung Dis 2013;17(6):719–727. ![]()
21. Centro Nacional de Vigilancia Epidemiológica y Control de Enfermedades, Dirección de Micobacteriosis. Mejora Participativa de los Sistemas Locales para detener la Tuberculosis, Jurisdicción Tijuana, Baja California. Enero – Febrero 2008 [cited 2015 Apr 9]. Available from: http://www.paho.org/mex/index.php?option=com_docman&task=doc_download&gid=95&Itemid=377
22. Fram SM. The Constant Comparative Analysis Method Outside of Grounded Theory. The Qualitative Report [Internet]. 2013 [cited 2015 Dec 18];18:1–25. Available from: http://nsuworks.nova.edu/cgi/viewcontent.cgi?article=1569&context=tqr
23. Glaser BG, Strauss AL. The discovery of Grounded Theory: Strategies for Qualitative Research. New Brunswick, USA: Aldine Transaction; 2006.
24. Corbin J, Strauss A. Basics of qualitative research: Techniques to developing grounded theory. 4th ed. Los Angeles, CA: Sage; 2008.
25. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3(2):77–101. ![]()
26. Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med 2009;36(5):452–7. ![]()
27. Zúñiga ML, Blanco E, Palinkas LA, et al. Cross-Cultural Considerations in the Recruitment of Latinos of Mexican-Origin into HIV/AIDS Clinical Trials in the US-Mexico Border Region: Clinician and Patient Perspectives. J Immigr Refug Stud 2010;8:241–260. ![]()
28. Muñoz FA, Servin AE, Kozo J, et al. A binational comparison of HIV provider attitudes towards the use of complementary and alternative medicine among HIV-positive Latino patients receiving care in the US-Mexico border region. AIDS Care 2013;25(8):990–7. ![]()
Appendix 1
University of California, San Diego (UCSD)
VCP-DOT Pilot Program Focus Groups
Dr. Richard Garfein
PATIENT FOCUS GROUP FACILITATOR GUIDE
Introduction
I appreciate your help with the consent forms and the brief survey. A few notes about our session today. This session will be recorded, but your name will not appear in any report or summary of the session. All of your comments are very important and we would like to give each person the opportunity to talk about their experiences or express their views. It is also important to remember that what is talked about here is confidential and that we respect everyone’s privacy and keep our conversation in this room.
Ok, now let’s get started …
People who work in health care know it is important to be able to help TB patients take their medications. Directly observing patients taking their medications has been shown to significantly improve adherence to treatment, but we are aware that this can be time-consuming and inconvenient for patients. We want to understand better whether we can use cell phone technology to remotely watch patients taking their medications.
I will now explain how face-to-face DOT is currently done and then I’ll explain how we think VCP-DOT can be done. (EXPLAIN FLOW DIAGRAM BRIEFLY TO PARTICPANTS).
VCP-DOT Procedures: Are they appropriate?
Let’s start by getting an idea of how familiar the members of our group are with using cell phones …
Q1. How often each day do you use your cell phone (for calls, texting, or other reasons)?
Q1.1 What experiences have you had using a cell phone to take a picture or video and send it to someone? Have you seen someone else do this?
Q2. If you were to receive a cell phone that can record video, what problems do you think you might have with using cell phones to send a video?
Q3. How do you think such problems could be overcome?
Q4. In what situations do you think VCP-DOT would not be good to use?
Q5. Will standard or VCP-DOT be more effective in helping patients to take all of their medications? Why? Why not?
Q6. If you were going to use the VCP-DOT what would make it easier for you?
Q6.1. Let’s say that you were instructed to take your TB medication at 1:00 in the afternoon, how hard would it be for you to find a place to record this process and send it to the nurse (by “hard” I mean finding a private place, finding the time to do it, etc)
Q6.2 Now what do you think would make it easier for you to do this?
VCP-DOT Advantages/Disadvatages
Q7. Let’s think about comparing the two kind of directly observed therapy, the standard way and then using cell phone video … In your opinion what advantages do cell phones have over standard DOT?
Q8. What disadvantages does VCP-DOT have compared with standard DOT?
Technical Advantages and Disadvantages of VCP-DOT
Q9. What cell phone features (display size, camera quality, keyboard size and layout, memory capacity, sound quality, unlimited minutes, etc.) would you like to see if you were going to try out this new process to send video information?
Q10. Are cell phones acceptable and a good option for patients?
Q11. Would it help patients remember to take their medication and send their video recordings if they received a reminder message on their phone everyday?
Final Thoughts – End of the Session
Q12. What other ideas do you think could help people use the cell phone for taking their TB meds? Perhaps something that we have not talked about yet, that may improve our ability to use this technology for medications?
End of Session
Conclusion: This concludes our focus group session. I very much appreciate your participation today. What we have learned from you is very important in order to know how to best implement the VCP-DOT Pilot program in our community.
Once again, thanks.
Appendix 2
University of California, San Diego (UCSD)
VCP-DOT Pilot Program Focus Groups
Dr. Richard Garfein
PROVIDER FOCUS GROUP FACILITATOR GUIDE
Introduction
I appreciate your help with the consent forms and the brief survey. Now we can begin the focus group discussion.
Our discussion will focus on the potential barriers and facilitators of using cell phones to record and send videos of patients self-administering their TB medications. Our purpose is to ask clinicians about their opinions on methods to overcome barriers with Video Cell Phone-Direct Observed Therapy (VCP-DOT) and to develop optimal procedures for delivering VCP-DOT. We are also asking patients in separate focus group discussions.
This session will be recorded, but your name will not appear in any report or summary of the session. All comments are very important and we would like to give each person the opportunity to talk about their experiences or express their views. It is also important to remember that what is talked about here is confidential and that we respect everyone’s privacy and keep our conversation in this room.
I will now compare how face-to-face DOT is currently done with how we think VCP-DOT can be done. (EXPLAIN FLOW DIAGRAM BRIEFLY TO PARTICPANTS).
VCP-DOT Procedures: Are they appropriate?
Q1. Which of these procedures do you think are appropriate? Which are inappropriate?
Q2. Do you see any procedures that will be difficult for the patient to follow?
Q3. Do you see any procedures that will be difficult for the TB Control staff to implement?
Q4. What modifications would you recommend to offset these difficulties?
Q5. What aspects of VCP-DOT are considered improvements/deficits compared to standard DOT?
Q6. What VCP-DOT procedures that I described would you change and how?
Adherence To VCP-DOT Treatment
Q7. Are there additional enhancements that can be made to the VCP-DOT protocol to improve the patients’ or TB Control staff’s ability to maximize treatment adherence or lower cost?
Q8. What other features (e.g., reminder messages, FAQs, live support) should be included to improve adherence and patient satisfaction?
Q9. What type of patient characteristics would make a patient a poor candidate for VCP-DOT?
Technical Issues
Q10. What are some of the technical problems you think may arise and what do you think we would need to address these?
Q11. Do you have any thoughts about cell phone devices and service providers features that will be necessary for the intervention to function effectively?
Q12. How much training do patients need to use video cell phones?
Cost
Q13. Do you think VCP-DOT will cost more or less than standard DOT and why?
Use in Other Countries
Q14. In your opinion, do you think this intervention could be adapted for use in a resource-limited country, such as Mexico?
Final Thoughts – End of the Session
Q15. What else comes to mind, perhaps something that we have not talked about yet, that may improve the VCP-DOT Pilot Program?
End of Session
Conclusion: This concludes our focus group session. I very much appreciate your participation today. What we have learned from you is very important in order to know how to best implement the VCP-DOT Pilot program in our community.
Once again, thanks.

