“The BUS Framework: A comprehensive tool in creating an mHealth App utilizing Behavior Change Theories, User-Centered Design, and Social Marketing”
“The BUS Framework: A comprehensive tool in creating an mHealth App utilizing Behavior Change Theories, User-Centered Design, and Social Marketing”
Sajani Patel1, Monisha Arya2,3,4
1School of Social Sciences, Rice University, Houston, Texas; 2Department of Medicine Section of Infectious Diseases, Baylor College of Medicine, Houston, TX; 3Department of Medicine Section of Health Services Research, Baylor College of Medicine, Houston, Texas; 4Center for Innovations in Quality, Effectiveness and Safety (IQuESt), Michael E. DeBakey VA Medical Center, Houston, Texas
Corresponding Author: sajani.patel@alumni.rice.edu
Journal MTM 6:1:39–45, 2017
INTRODUCTION
Despite the explosion of health-related mobile applications (apps) – now numbering more than 43,0001 – few are widely used. One quarter of all apps downloaded are only used once.2 Amongst apps that help people manage their health, most are only downloaded fewer than 500 times, and only five apps account for 15% of all health app downloads.2 However, research has shown that when they are used, health apps are successful at improving the user’s health outcomes and preventing disease.3,4 Despite these successes of health apps, they are still not used to their fullest potential. A national survey found that while 58% of adults own a smart phone only half of these adults have apps on their phones.5,6 In fact, only one in three app users has ever downloaded an app that helps track or manage health.6 While health apps are not currently widely used, they are growing in popularity and could be an opportune platform to deliver health promotion campaigns. For this health promotion platform to be optimized, it is important that end-users are engaged in the health app development – a step that has been sometimes neglected in the health app development process to date.3
KEY INGREDIENTS FOR SUCCESSFUL UPTAKE AND USE OF HEALTH APPS
There may be several reasons that health app uptake has been disappointingly low. It is possible that the low uptake and use of health apps may be due to deficiencies in app design and a lack of app evaluation. Muessig suggests there is a lack of use of social marketing principles in app development.7 Additionally, Riley highlights the limited use of principles of behavior change theories in app development.8 Lastly, McCurdie notes that app development does not always use principles of user-centered design.3 Using these principles synergistically could help create a health app that focuses on and engages the end-user while successfully affecting health behavior change.
Behavior Change Theories
Health promotion specialists use behavior change theories to develop health campaigns for target audiences. These theories evaluate environmental, social, and personal factors (e.g. norms, attitudes, and beliefs) that may be influencing health behaviors.9 There are many different theories; each has its own set of constructs that influence behavior change. Three commonly used theories are Health Belief Model, Theory of Planned Behavior, and Social Cognitive Theory (See Table 1).9 Each theory can stand alone or constructs from multiple theories can be combined and tailored to best fit the campaign’s and the audience’s needs.
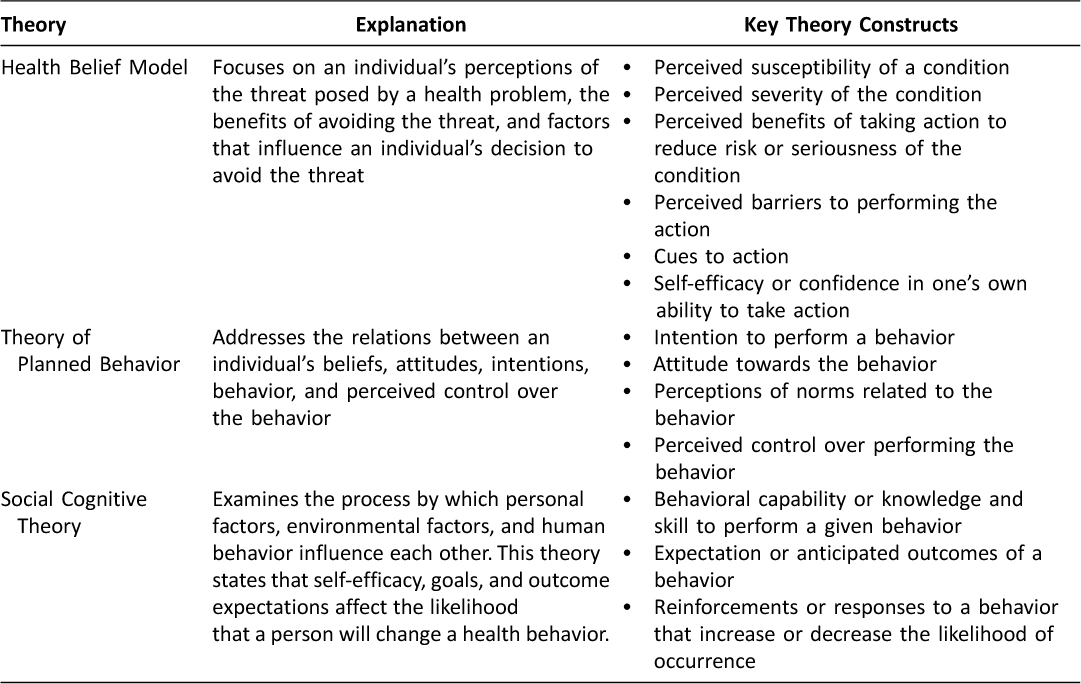
Table 1: Behavior change theories and their constructs, adapted from Theory at a Glance: A Guide for Health Promotion Practice.9
User-Centered Design
User-centered design (UCD) is an iterative design process that engages the end-users throughout product development. UCD analyzes the usability, usefulness, and fit of a technology in the end-user’s everyday life.10 When using this design process, the designer must ensure that the end-user is able to use the final product as intended, and can learn how to use it with minimal effort.11 Interventions that use UCD have a greater likelihood of achieving end-user engagement and being effective.3 UCD ensures the product creates sustained and positive behavior change.3 UCD can be especially beneficial in creating usable and sustainable health apps that account for end-users’ needs and preferences. See Figure 1 for a UCD model.
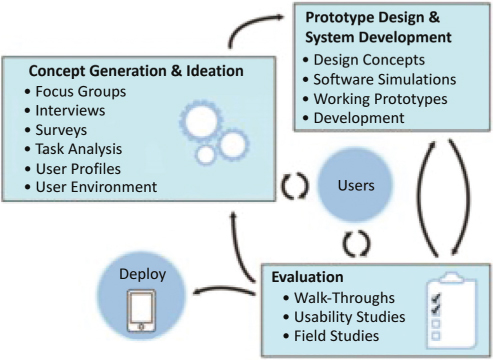
Figure 1: The User-Centered Design Process. (Adapted from McCurdie et al.)3
Social Marketing
Social marketing adopts traditional marketing principles to influence behaviors that improve health.12 It is most successful when used as a research-driven process that utilizes end-user feedback to create a tailored campaign for a specific audience.12 Social marketing is critical when planning health campaigns because it examines the viewpoint of the audience by incorporating the “Four P’s of Marketing.” These Four P’s are: product, price, place, and promotion.12 See Table 2 for how the Four P’s could be operationalized for health apps.
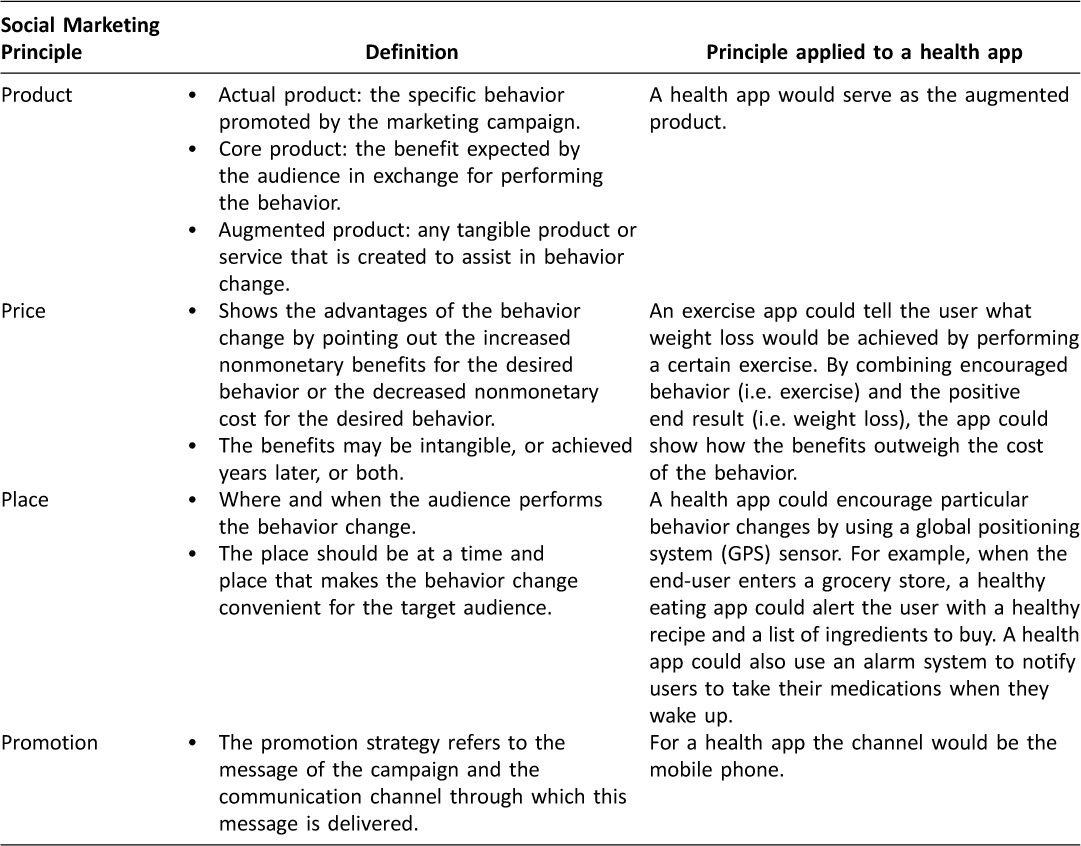
Table 2: The Four P’s of Social Marketing applied to a health app19
THE BUS FRAMEWORK: A COMPREHENSIVE TOOL FOR CREATING HEALTH APPS
The success of health apps may be improved by utilizing the BUS Framework, which incorporates principles from Behavior change theories, UCD, and Social marketing, or BUS. Figure 2 illustrates an app development framework incorporating all three of these to maximize app effectiveness. App creation should employ both quantitative and qualitative research methods. For example, quantitative methods could include surveying end-users about their health needs and their existing health knowledge, attitudes, and behaviors. Qualitative methods could include end-user interviews or focus groups for more in-depth feedback on health app prototypes.
Steps for Health App Creation
1) Situational Analysis
Performing situational analysis is the first step in app development. This analysis includes identifying the health problem, the target population (i.e., the campaign end-users), the behavioral determinants of the health problem, and the campaign partners and stakeholders. Identification of the health problem includes reviewing existing data on the health of a specific population and understanding aspects of the health problem.13 The target population should be narrowed down to a group of people with common characteristics (i.e. attitudes, demographics, patterns of behavior).13 Such audience segmentation is necessary to create a more homogenous target population with more similar needs. Campaigns that target broad populations, such as “adults”, are less successful because of the diversity of knowledge, attitudes and health behaviors in this large of a population.13 Also, successful campaigns should target determinants of behaviors (i.e. barriers and facilitators) that influence the health problem of interest in the target population.14,15 As noted in the Institute of Medicine report, Speaking of Health: Assessing Health Communication Strategies for Diverse Populations, “the more one knows about the determinants of a given behavior, the more likely it is that one can develop an effective communication intervention to reinforce or change that behavior.”16
After identifying the target audience and specifying the targeted health problem, it is important to identify and include partners and stakeholders to ensure that successful app creation and buy-in will occur. Partners are those who will support and promote the health campaign and may be advocates for the health issue. For example, the American Sexual Health Association could be a partner for a sexually transmitted disease (STD) testing campaign encouraging testing among female college freshmen. Stakeholders are third-party entities who may benefit from the campaign’s success. For example, stakeholders could be pharmaceutical companies who market drugs to treat STDs, university health centers that provide STD testing to college students, and financial investors in the app.
2) Concept Generation and Prototype Design
After the health problem has been identified through situational analysis, the concept for the campaign should be selected. For the example given above, the campaign’s concept would be increasing STD testing. The campaign developers should conduct surveys and interviews or focus groups with members of the target audience to understand their barriers and facilitators to STD testing. Based on these findings, constructs of behavior change theories can be utilized to design a prototype – a preliminary version of the final app – that meets the needs of the end-users. For example, if end-users are not being STD tested because they forget, the “cue to action” construct from the Health Belief Model could be incorporated in the app design to address this barrier. This could include the app sending the user a notification for her annual STD test. If end-users do not know where to get an STD test, the construct of “perceived control” from the Theory of Planned Behavior could be applied, and the app could use geo-sensing to show the user a map with nearby STD testing facilities. Finally, if end-users do not know if they should be STD tested, “behavioral knowledge” from Social Cognitive Theory can guide the app developers in designing the app to provide users with the latest STD testing recommendations that are specific to them. The end result of this step could include picture mock-ups of the app screens and an outline of intended app functions.
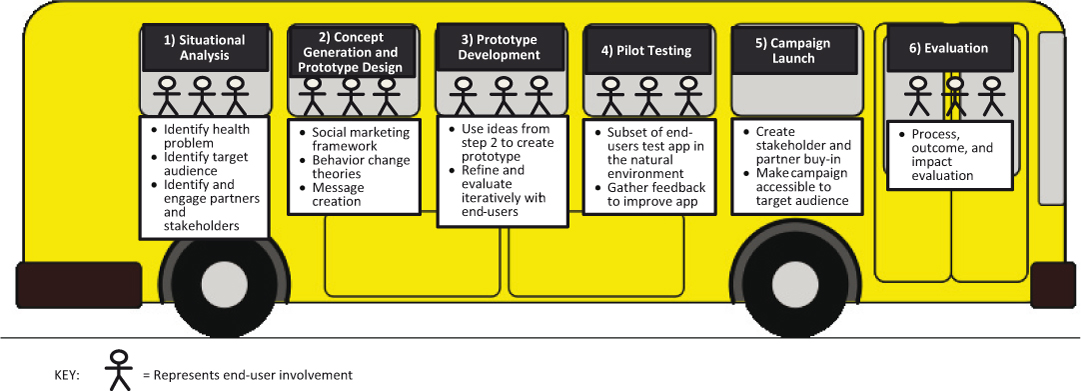
Figure 2: BUS Framework: Steps for health app creation
3) Prototype Development
The app prototype should be created using the design framework created in Step 2. End-users should be engaged to test progressive versions of the prototype through walk-throughs and usability testing.3,11 Walk-throughs entail guiding a small sample of end-users through all aspects of the prototype. The developers should present the app to the end-users to “find anomalies, improve the software product, [and] consider alternative implementations.”17 For example, in the STD testing app users would give developers feedback on whether the app should have its own calendar for testing reminders or if the app should connect to the existing calendar on the user’s phone. End-user feedback could also reveal end-user preferences on the size of the radius of nearby STD testing clinics in the app’s STD testing facilities map. Finally, usability testing should be done. This involves giving the prototype to the end-user and observing their ability to navigate it without aid from the developers.
4) Pilot Testing
The app should be given to a sample population of the end-users. These end-users should be given access to the app and use it in their everyday life for a defined period of time. This would allow the developers to ensure that the app is applicable in the end-users’ natural environments. At the end of this period, end-users would give feedback to the campaign developers about their experience using the app and any input they have on improving it. This feedback can be gathered through surveys, interviews, and/or focus groups. End-user feedback allows the development team to see which aspects of the health app are working and which need to be changed to be more effective. Based on the results of the feedback, further iterations of the prototype can be created if necessary.
5) Campaign Launch
Once the final functioning app has been created and successfully pilot tested, it should be pitched to the stakeholders and partners in order to create buy-in for the final product. Should the stakeholders buy into the app, they will be more likely to provide support for the campaign, which could result in additional resources to launch the campaign to a wider audience and to make the campaign successful. At this point, the campaign can be launched and made accessible to the target audience through advertising, promotion by stakeholders and partners, and media reporting.
6) Evaluation
The final, and often overlooked, step is campaign evaluation. There are three types of evaluation13 – process, outcome, and impact – all of which could use quantitative and qualitative methods to obtain feedback from all parties involved throughout the campaign development process (i.e., target audience, campaign developers, stakeholders, and partners). Process evaluation assesses if the health app was developed and implemented successfully. This evaluation should determine if the project was completed in the allotted timeframe, if the selected stakeholders and partners were actively involved in the project, if the app was developed within the budget, if the app was sufficiently publicized, if the target audience successfully downloaded the app, and if the target audience used the app. Outcome evaluation focuses on end-users’ perceptions and interpretations of the campaign and the immediate behavior change that resulted from the health app. This evaluation should include assessing changes in knowledge, attitudes, and behaviors related to the targeted health problem. For example, outcome evaluation of the STD testing app would include determining if STD knowledge improved because of the app, if end-users were encouraged to get STD tested because of the app, and if end-users had any barriers to using the app (e.g. the end-user was embarrassed about receiving calendar reminders about STD testing). Finally, impact evaluation measures the long-term, broader effect the campaign has on the end-users. This could include getting periodic STD testing data from university health centers over the duration of the campaign.
CONCLUSION
Smartphones and mobile applications are increasing in popularity. However, this technology is being underutilized for health, despite its potential to engage patients and influence positive health behavior changes. Successful health apps should be designed using the principles of behavior change theories, user-centered design, and social marketing as illustrated in the BUS Framework. Doing so would also help achieve the U.S. Department of Health and Human Services Healthy People 2020 objective of increasing the use of mobile technologies for health.18 Designing campaigns based on the BUS Framework could be a way to effectively use this burgeoning technology for creating positive behavior change and improving patient health.
Acknowledgements
The authors would like to thank Dr. Richard Street, Ms. Disha Kumar, and Ms. Ashley Phillips for their thoughtful comments and editorial assistance on the manuscript. Additionally, the authors would like to thank Dr. Daniel Murphy for guiding the development of Figure 2. This research was supported by the Rice University Janus Award (Sajani Patel) and the Rice University Social Sciences Undergraduate Research Enterprise (Sajani Patel), both undergraduate research scholarships. This research was also supported by an NIH-funded program and the National Institute of Mental Health of the National Institutes of Health under Award Number K23MH094235 (PI: Arya). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Rice University. This work was supported in part by the Center for Innovations in Quality, Effectiveness and Safety (#CIN 13-413). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. We have no conflict of interests to disclose. This paper or papers similar to it have not been submitted or published previously by any of the authors.
References
1. Sifferlin A. Bad News About Your Favorite Health Apps: They Don’t Work: Time Magazine; 2013 [cited 2016 May 5]. Available from: http://healthland.time.com/2013/10/31/bad-news-about-your-favorite-health-apps-they-dont-work/.
2. Leger B. 26% of mobile apps downloaded in 2010 were used just once: Localytics; 2011 [cited 2016 May 5]. Available from: http://info.localytics.com/blog/first-impressions-26-percent-of-apps-downloaded-used-just-once.
3. McCurdie T, Taneva S, Casselman M, Yeung M, McDaniel C, Ho W, et al. mHealth Consumer Apps: The Case for User-Centered Design Advancing Safety in Medical Technology: Horizons. 2012.
4. Handel MJ. mHealth (mobile health)-using Apps for health and wellness. Explore. 2011;7(4):256–61. ![]()
5. Pew Research Center. Cell Phone and Smartphone Ownership Demographics 2014 [cited 2016 May 5]. Available from: http://www.pewinternet.org/data-trend/mobile/cell-phone-and-smartphone-ownership-demographics/.
6. Purcell K. Half of adult cell phone owners have apps on their phones 2011 [cited 2016 May 5]. Available from: http://www.pewinternet.org/files/old-media/Files/Reports/2011/PIP_Apps-Update-2011.pdf.
7. Muessig KE, Pike EC, Legrand S, Hightow-Weidman LB. Mobile phone applications for the care and prevention of HIV and other sexually transmitted diseases: a review. Journal of medical Internet research. 2013;15(1):e1. ![]()
8. Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Translational behavioral medicine. 2011;1(1):53–71. ![]()
9. National Cancer Institute. Theory at a Glance: A Guide for Health Promotion Practice 2005 [cited 2016 May 5]. Available from: http://www.sneb.org/2014/Theory at a Glance.pdf.
10. Poole ES. HCI and mobile health interventions: How human-computer interaction can contribute to successful mobile health interventions. Translational behavioral medicine. 2013;3(4):402–5. ![]()
11. Abras C, Maloney-Krichmer D, Preece J. User-Centered Design. Encyclopedia of Human-Computer Interactions. 2004.
12. Centers for Disease Control and Prevention. What is Health Communication? 2011 [cited 2016 May 5]. Available from: http://www.cdc.gov/healthcommunication/healthbasics/whatishc.html.
13. National Cancer Institute. Making Health Communication Programs Work 2004 [cited 2016 May 5]. Available from: http://www.cancer.gov/publications/health-communication/pink-book.pdf.
14. Fishbein M, Cappella JN. The role of theory in developing effective health communications. Journal of Communication. 2006;56:S1–S17. ![]()
15. Randolph W, Viswanath K. Lessons learned from public health mass media campaigns: marketing health in a crowded media world. Annu Rev Public Health. 2004;25:419–37. ![]()
16. Institute of Medicine. Speaking of Health: Assessing Health Communication Strategies for Diverse Populations. Washington, DC: The National Academies Press; 2002.
17. IEEE Computer Society. IEEE Standard for Software Reviews and Audits 2008 [cited 2016 May 5]. Available from: http://dis.unal.edu.co/~icasta/ggs/Documentos/Normas/1028-2008.pdf.
18. Office of Disease Prevention and Health Promotion. Healthy People 2020 2015 [cited 2016 May 5] Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/health-communication-and-health-information-technology/objectives.
19. Lee N, Kotler P. Social Marketing: Quick Reference Guide 2008 [cited 2016 May 5]. Available from: file:///C:/Users/shp2/Desktop/Downloads/lee_handout_1348.pdf.

