Current Use of Smartphone and Tablet Applications in Orthopaedic Surgery Residency
Current Use of Smartphone and Tablet Applications in Orthopaedic Surgery Residency
Joshua C. Luginbuhl MD1, Joey P. Johnson MD2, Anthony J. Boniello MD3, Mary K. Mulcahey MD4
1Joshua C. Luginbuhl, M.D., is an orthopaedic resident at Temple University Hospital in Philadelphia, Pennsylvania; 2Joey P. Johnson, M.D., is an orthopaedic trauma fellow at Brown Alpert Medical School in Providence, Rhode Island; 3Anthony Boniello, M.D., is an orthopaedic resident at Drexel University College of Medicine/Hahnemann University Hospital in Philadelphia, Pennsylvania; 4Mary K. Mulcahey, M.D., is an Associate Professor of orthopaedic surgery at Tulane University School of Medicine, New Orleans, Louisiana.
Corresponding Author: joshluginbuhl@gmail.com
Journal MTM 7:1:32–39, 2018
Background: In orthopaedic surgery residency, traditional methods of education are being challenged by more technologically advanced modalities, specifically smartphone and tablet applications. Although these tools have become increasingly popular among orthopaedic surgeons, uncertainty remains about the widespread use of applications in orthopaedic residency.
Aims: This study aims to evaluate the perception of orthopaedic residents regarding the use of applications to support their education and clinical decision-making.
Methods: An anonymous, 25 question survey regarding the use of clinical and educational applications during residency training was distributed to 50 orthopaedic residents at two different ACGME-accredited programs. Statistical analysis was performed using two tailed t-tests for analysis of means, and chi-squared tests of independence of categorical variables, with significance defined as a p<0.05 a priori.
Results: Thirty-seven residents (Response Rate: 74%) completed the survey. Most residents use a specific free orthopaedic reference application on a weekly basis (86.1%). Thirty-six residents (97.3%) believe that there is an educational benefit from medical applications, however, the majority of residents (54.05%) believe that senior physicians look down upon the use of applications during clinical practice. Over 90% of residents agree that the cost of an application affects the decision to download and use it.
Conclusion: Most orthopaedic surgery residents use a wide variety of applications on a daily basis. Despite the increasing role of applications, the perception among residents that senior physicians look down upon the use of applications could be a barrier to widespread implementation.
Keywords: Orthopedics, smartphone, residency, technology, education
Introduction
The American Board of Orthopaedic Surgery (ABOS) was established in February 1934 with the intention of creating a universal standard of education. By 1936, the ABOS instituted the first formal requirements for certification in order to monitor physician quality and to ensure public trust.1 In addition to the certification examination administered by the ABOS, the American Academy of Orthopaedic Surgeons (AAOS) developed the Orthopaedic In-Training Examination (OITE) to assess whether each orthopaedic residency program was attaining its educational goals.
The establishment of the ABOS and the implementation of the OITE by the AAOS, led to high expectations for the quality of orthopaedic residency education. Previous studies have evaluated the types of resources that residents use to prepare for standardized examinations, specifically, traditional methods such as didactic lectures, case conferences, and textbooks.2 However, like many fields of medicine, orthopaedic residency education has changed rapidly as advancements in technology, specifically smartphone applications, have evolved.
With the advent of smartphones and tablets, physicians can now access a large amount of information from a single device through downloadable applications. A survey was distributed to all Accreditation Council for Graduate Medical Education (ACGME) training programs in 2011 to evaluate the prevalence of smartphone use across medical specialties. The study found that over 85% of respondents, which included residents, fellows, and attendings, owned a smartphone capable of accessing medical applications.3 Along with widespread smartphone use, applications have become integrated in many medical specialties. In urology, applications exist that allow patients to record intake and output and provide a way for practicing urologists to access the Oxford Handbook of Urology.4 In dermatology, there are over 200 applications with uses that range from general dermatology reference to educational aid.5,6 Likewise, there are more than 340 applications available for ophthalmology, ranging from educational flashcards to virtual surgery applications that detail the steps of common operations.7 The number of applications available for educational and clinical purposes is rapidly expanding with more applications being targeted at individual specialties, including orthopaedic surgery.8,9 From 2010 to 2014, orthopaedic residents increased their use of smartphone applications in the clinical setting from 60% to 84%, whereas attending use increased from 41% to 61%.10 During this same time period, 70% of orthopaedic surgeons believed their institution/hospital should support mobile device use.10
Despite the rapid expansion and use of available medical applications, questions remain about their safety, validity, and role in educational and clinical settings.11–14 Several recent studies have demonstrated that some orthopaedic applications, such as those that measure gait, range of motion, and degree of spinal deviation in scoliosis, are as accurate as more traditional measuring devices.15–20 While many applications have been thoroughly evaluated for accuracy, there remains a paucity of standardized testing protocols creating a wide variability in the usefulness, quality and accuracy of available applications. Ongoing uncertainty therefore exists regarding how the advancement of applications will affect traditional teaching in orthopaedic training programs. The objective of this study was to evaluate the perception of orthopaedic surgery residents regarding the use of educational and clinical smartphone and tablet applications to support their training and decision making.
Methods
Survey
An anonymous 25-question online survey was formulated focusing on questions about frequency of application use, common barriers encountered, and opinions regarding application use during orthopaedic surgery residency (Appendix). The survey was distributed via Survey Monkey (SurveyMonkey Inc., Palo Alto, California, USA) to all current orthopaedic surgery residents at two university-affiliated residency programs in the United States (50 residents total). Demographic variables collected included current postgraduate-year and residency program. Eleven questions regarding use of applications and opinions toward application use were answered by selecting a categorical variable or by using a five-point Likert scale (“disagree”, “somewhat disagree”, “neutral”, “somewhat agree”, “agree”), while the remaining questions were answered by selecting a categorical variable (Appendix A) Participation was anonymous and voluntary, however, follow-up emails were sent to residents at 2 and 4 weeks to encourage more participation.
Analysis
Statistical analysis was performed using two tailed t-tests for analysis of means, and chi-squared tests of independence of categorical variables, with significance defined as a p<0.05 a priori. Outcome variables were statistically analyzed using data analysis software (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP).
IRB Approval
This study (IRB ID: 1609004847) was approved by the Institutional Review Board (IRB) at the principal investigator’s institution* and complies with all relevant federal, state, and local regulations (* the PI was faculty at Drexel University College of Medicine at the time of IRB approval and initial manuscript submission, but is now a practicing physician at Tulane University School of Medicine).
Results
Use of applications
Thirty-seven residents (74% response rate) from the two orthopaedic surgery residency programs completed the survey. The number of applications and frequency of use varied, with the majority of residents using 1 to 4 applications (78.4%), 1 to 4 times per day (81.1%) (Figure 1). Thirty-two of the residents who responded (86.1%) use a specific free orthopaedic surgical reference guide application on a weekly basis. Smartphones are used more often than tablets for both educational (89.7%) and clinical (78.8%) purposes.
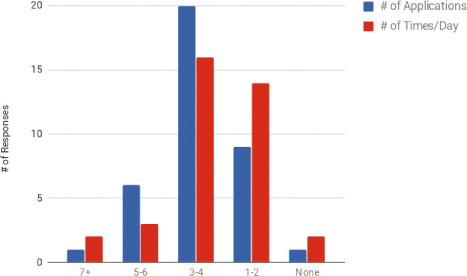
Figure 1: Frequency of educational and clinical application use among orthopaedic residents.
Opinions about applications
Thirty-six residents (97.3%) believe that medical applications provide an educational benefit and that they allow for improved efficiency in an educational or clinical setting. Only one resident (2.7%) believes that applications cannot be trusted to provide information for clinical decisions. Furthermore, four residents (10.8%) think that applications do not play an important role in clinical decision making (Figure 2). Two residents (5.4%) believe that their colleagues depend too much on applications. Twenty residents (54%) somewhat agree or agree that senior physicians “look down upon” application use during clinical practice. In addition, 17 residents (45.9%) believe that patients think less of a physician who uses applications during a clinical encounter, while 13 residents (35.1%) do not have this perception (Figure 3).
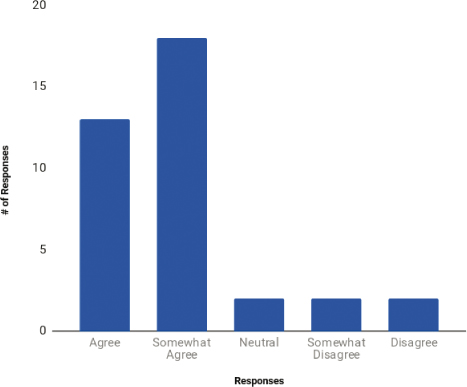
Figure 2: Resident response to “I think applications play an important role in clinical decision making.”
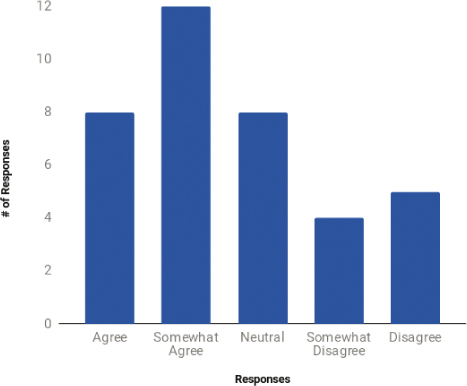
Figure 3: Resident response to “I feel that older physician look down on application use during clinical practice.”
There were no difference between junior residents (PGY1-3) and senior residents (PGY4-5) in trusting applications for clinical decisions (86.9% versus 76.8%, p=0.236, CI: -31.0-31.0), believing applications play an important role in the clinical setting (86.9% versus 78.6%, p=0.482 CI: -44.6-44.6), noticing an educational benefit of applications (100% versus 92.8%, p=0.250, CI: -22.8-22.8), believing that applications make them more efficient (100% versus 92.8%, p=0.213, CI: -21.0-21.0), and believing peers rely too much on applications in the clinical setting (21.7% versus 42.8%, p=0.410, -95.9-95.8) (Table 1).
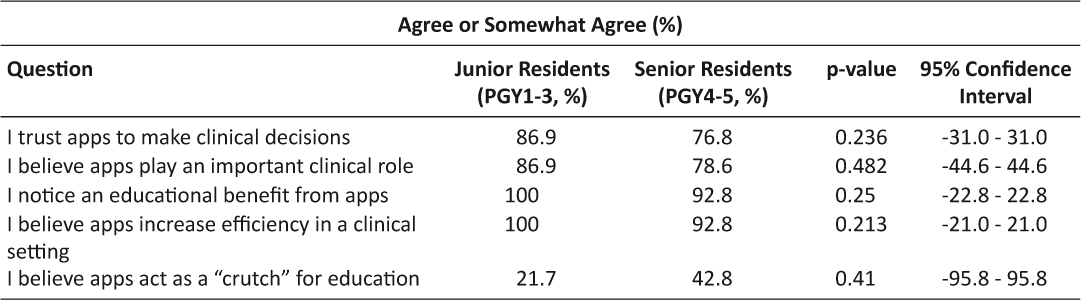
Table 1: Perception of the value of smartphone application use among junior (PGY1-3) and senior (PGY4-5) orthopaedic surgery residents.
Factors influencing the use of applications
Thirty-four orthopaedic surgery residents (91.9%) agree that cost affects the decision to download and/or use an application and 22 respondents (59.4%) were willing to pay between $1-$10. Poor utility and design, along with high cost, were the most significant personal barriers to application use.
Discussion
Smartphone and tablet technology have become pervasive throughout society and reshaped the workplace across a variety of disciplines, including medicine. Applications designed for smart phone use are now common place in hospitals, with specialty-specific tools being used as a routine part of patient care.3,4,5,7,9 This study demonstrates that the majority of orthopaedic surgery residents surveyed use smart phone, or tablet applications in a clinical setting. Furthermore, only one resident surveyed did not trust the information provided in these applications and only two residents surveyed believed that their colleagues are too dependent upon applications. There were no statistically significant differences between junior and senior residents with regards to application use, or attitudes toward application use. Eighty-four percent of residents surveyed reported using the same clinical application on a daily basis.
With the rapid growth of technology in society and medicine, an increasing number of specialty-specific medical applications have become available including numerous related to orthopaedic surgery.3,4,8,9 Many of these applications have been shown to be accurate, and several are supported by subspecialty societies.15 Despite this, there is a paucity of literature describing the appropriate use of educational and clinical applications, and few professional societies have issued formal statements or policies on their use.8
The educational guidelines for orthopaedic residency programs have become increasingly stringent in recent years, in an effort to standardize the quality of training provided to future orthopaedic surgeons.1 As the requirements become more exacting, the amount of time that residents are allowed to devote to patient care continues to decrease.21,22 In 2003 and again in 2011, the ACGME mandated increasingly strict guidelines limiting the amount of time residents can spend in the hospital taking care of patients, and learning in a clinical setting. By providing residents with a more facile way of accessing educational materials, applications may improve the ability of residents to augment the education they may be missing as their time in the hospital is increasingly limited.3 Additionally, applications that are focused on patient care, may help residents streamline the more time consuming aspects of clinical work, allowing them to spend more of their already limited time in the hospital actively engaged in educational endeavors. Although smartphone applications can improve educational and patient care opportunities, our study showed that more than half of our respondents believe that attending orthopaedic surgeons do not agree with frequent use of these tools.
The present study is limited by its descriptive nature, and survey-based methodology. Additionally, the small group of residents (n = 50) surveyed may limit extrapolating broad generalizations of national and temporal trends. Conclusions extrapolated to national trends are limited as the surveys were completed by two urban teaching hospitals. It is possible that rural programs in the same state or region may have differing opinions regarding the role of applications in educational and clinical settings. A broader based survey querying a diverse group of programs around the country would be necessary to make more definitive conclusions of national trends. Additionally, we only surveyed trainees, thus we cannot comment specifically on the opinions of senior surgeons with regard to the use of smartphone applications. The present study did however experience a high response rate (74%). While conclusions should not be made on national trends, the study does demonstrate a substantial need to quantify the current usage of, as well as the present need to study the efficacy, safety, and accuracy of these applications.
Conclusion
This study adds to the discussion of how technology can be used in the current medical and educational landscape in orthopaedic residency training programs. The vast majority of residents surveyed use applications on a regular basis and trust the content they provide. There were no significant differences in the attitudes towards applications between junior and senior residents. However, there was a perception by the majority of respondents that senior orthopaedic surgeons look down upon the use of applications. The use of applications by orthopaedic surgeons and the number of applications available continue to increase.10 The current study speaks to the potential utility of applications in orthopaedic training; however, further studies are needed to determine the optimal use of applications in clinical and educational orthopaedic settings.
References
1. The History of the American Board of Orthopaedic Surgery. c2016. Chapel Hill (NC): The American Board of Orthopaedic Surgery; [accessed 2016 Aug 13]. https://www.abos.org
2. Miyamoto RG, Klein GR, Walsh M, et al. Orthopedic surgery residents’ study habits and performance on the orthopedic in-training examination. Am J Orthop 2007;36:185–188.
3. Franko OI and Tirrell TF. Smartphone app use among medical providers in ACGME training programs. J Med Sys 2012;36:3135–3139. ![]()
4. Abboudi H and Amin K. Smartphone applications for the urology trainee. BJU Int 2011;108:1371–1373. ![]()
5. Brewer AC, Endly DC, Henley J, et al. Mobile applications in dermatology. JAMA dermatol 2013;149:1300–1304. ![]()
6. Wolf JA, Moreau JF, Akilov O, et al. Diagnostic inaccuracy of smartphone applications for melanoma detection. JAMA dermatol 2013;149:422–426. ![]()
7. Zvornicanin E, Zvornicanin J, and Hadziefendic B. The use of smartphones in ophthalmology. Acta Inform Med 2014;22:206. ![]()
8. Myutan K, Marcus L, Georgia L, et al. Surgical Smartphone Applications Across Different Platforms Their Evolution, Uses, and Users. Surg Innov 2014;21:427–440: ![]()
9. Franko OI. Smartphone apps for orthopaedic surgeons. Clin Orthop Relat Res 2011;469:2042–2048. ![]()
10. Andrawis JP, Muzykewicz DA, and Franko OI. Mobile Device Trends in Orthopedic Surgery: Rapid Change and Future Implications. Orthopedics 2016;39:51–56. ![]()
11. Ozdalga E, Ozdalga A, and Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res 2012;14:128. ![]()
12. Skomorowski M, Jordan K, Schroeder K, et al. Resident impressions of the clinical utility and educational value of the iPad. J Mob Technol Med 2013;2:21–26. ![]()
13. Wong SJ, Robertson GA, Connor KL, et al. Smartphone apps for orthopaedic sports medicine–a smart move? BMC Sports Sci Med Rehabil 2015;7:1. ![]()
14. Buijink AW, Visser BJ, and Marshall L. Medical apps for smartphones: lack of evidence undermines quality and safety. Evid Based Med 2013;18:90–92. ![]()
15. Jenny JY. Measurement of the knee flexion angle with a smartphone-application is precise and accurate. J Arthroplasty 2013;28:784–787. ![]()
16. Jenny JY, Bureggah A, and Diesinger Y. Measurement of the knee flexion angle with smartphone applications: which technology is better? Knee Surg Sports Traumatol Arthrosc 2015;24:1–4.
17. Werner, BC, Holzgrefe RE, Griffin JW, et al. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J Shoulder Elbow 2014;23:275–282. ![]()
18. Furrer M, Bichsel L, Niederer M, et al. Validation of a smartphone-based measurement tool for the quantification of level walking. Gait Posture 2015;42:289–294. ![]()
19. Meislin, MA, Wagner ER, and Shin AY. A Comparison of Elbow Range of Motion Measurements: Smartphone-Based Digital Photography Versus Goniometric Measurements. J Hand Surg 2016;41:510–515. ![]()
20. Franko OI, Bray C, and Newton PO. Validation of a scoliometer smartphone app to assess scoliosis. J Pediatr Orthop 2012;32:72–75. ![]()
21. Camp CL, Martin JR, Karam MD, et al. Orthopaedic Surgery Residents and Program Directors Agree on How Time Is Currently Spent in Training and Targets for Improvement. Clin Orthop Relat Res 2016;474:915–925. ![]()
22. Mir HR, Cannada LK, Murray JN, et al. Topics in Training Opinions of Resident Duty Hours. J Bone Joint Surg 2011;142:1–9.
Appendix A
Survey:
PGY Year
- 1
- 2
- 3
- 4
- 5
- 6/attending
Sex
- M
- F
Affiliation
- Brown
- Drexel
Which of the following do you use most for applications related to education?
- Smartphone
- Tablet
Which of the following do you use most for applications related to clinical practice?
- Smartphone
- Tablet
How many applications do you use for education or as a clinical tool?
- None
- 1−2
- 3−4
- 5−6
- 7+
On average, how many days/week do you use applications?
- None
- 1−2
- 3−4
- 5−6
- 7
On average, how many times/day do you use applications?
- None
- 1−2
- 3−4
- 5−6
- 7+
I notice an education benefit from medical applications
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
Applications allow me to be more efficient in a clinical or educational setting.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
I believe that applications act as a crutch for education.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
I trust basing medical decisions on information provided by an application.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
I think my colleagues depend on applications too much.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
I think applications play an important role in clinical decision making.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
I feel that older physicians look down on application use during clinical practice.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
I feel that patients think of a physician differently if they use an application during a clinical encounter.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
I feel comfortable using my smartphone/tablet.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
The amount of memory an application uses affects my decisions to us/download it.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
I use an application less if it uses a significant amount of battery life.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
The cost of an application affects my decision to download/use it.
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
What is the maximum price range you would be willing to pay for an education/clinical application?
- 0
- 1−5
- 6−10
- 11−15
- 15+
The presence of advertisements deters me from using certain applications
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
Negative stigma affects how much I use my application in a clinical setting
- Disagree
- Somewhat disagree
- Neutral
- Somewhat agree
- Agree
Rank in order (1-most, 6-least), the most significant personal barrier to application use
- High cost
- High memory use
- Poor design
- Poor utility
- Negative stigma
- Advertisements
Please select which application you use on a weekly basis
- QxMD
- Endnote
- iNotes
- MedCalc
- Epocrates
Remote EMR access applications
- OpTech Live
- Traumaline
- SLIC
- Mobile Coder Orthopedics
- AO Surgery Reference
- Orthopedics Terminology
- Orthopedics Glossary
- Orthopedics Today Helio for iPhone
- Learning Orthopedics Quiz
- Goniometer pro
- Orthopedics Encyclopedia
- iDo Now Orthopedics
- Muller AO Classification of Fractures
- Case Files Orthopedic Surgery
- ICJR
- RadTechPro
- SportsMed
- OrthoAnatomy
- OrthoEvent
- OrthoKeys
- Aesculp Spine Cervical
- OrthoRef Lite
- Acta Orthopaedics Journal
- Multiplier
- Bone Ninja
- Knee Goniometer
- Orthopaedics Today Europe
- Bone Feed
- Spinal News International
- Sports Health
- OITE Strategy
- Surgical Instrument Quiz
- MSK Injections
- Cyber PT Tx
- Osteoporosis by AZoMedical
- OrthoMind
- Electromyography Multilingual
- BoneCase
- TherapyWhiz
- BoneTest Miscellaneous
- OrthoRef
- UCSF MSK Exam Tutor
- Cobb Reader
- ShoulderDox
- Orthoclass
- Rotho Traumapedia
- Orca MD Series
- DrawMD Orthopedics
- Orthopedic Patient Education
- CORE
- iOrtho+
- Realworld Orthopedics
- T&O Curriculum
- Tumorpedia
- MyATLS Trauma
- Insights Orthopedics

