Designing a WIC App to Improve Health Behaviors: A Latent Class Analysis
Designing a WIC App to Improve Health Behaviors: A Latent Class Analysis
Sylvia H. Crixell PhD, RD1, Brittany Reese Markides MS, RD2, Lesli Biediger-Friedman PhD, MPH, RD3, Amanda Reat MS, RD2, Nicholas Bishop PhD4
1Nutrition and Foods Professor, School of Family and Consumer Sciences, Texas State University, San Marcos, Texas; 2Nutrition and Foods Lecturer, School of Family and Consumer Sciences, Texas State University, San Marcos, Texas; 3Nutrition and Foods Assistant Professor, School of Family and Consumer Sciences, Texas State University, San Marcos, Texas; 4Family and Child Development Assistant Professor, School of Family and Consumer Sciences, Texas State University, San Marcos, Texas
Corresponding Author: scrixell@txstate.edu
Journal MTM 7:2:7–16, 2018
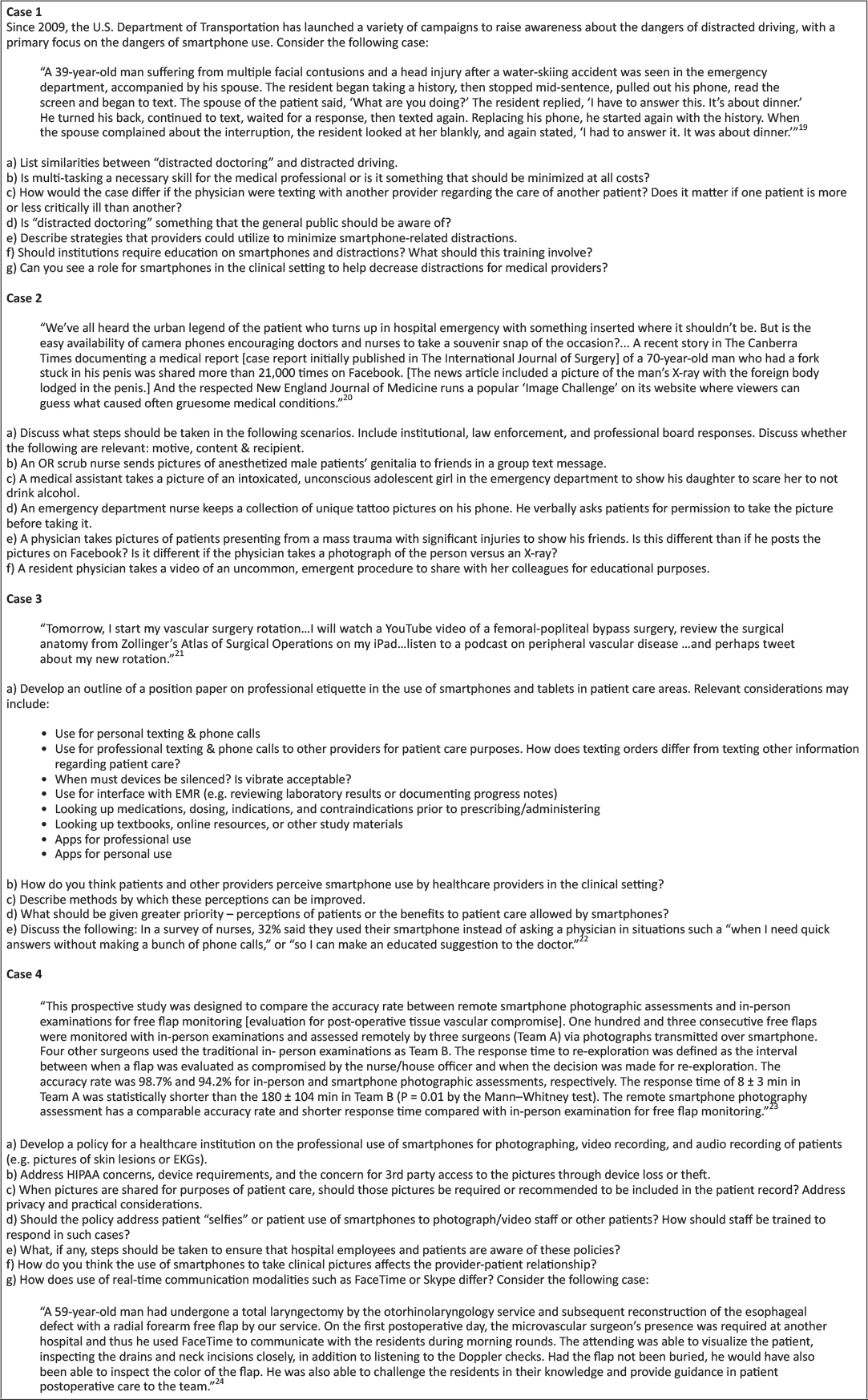
Background: Smartphone apps have potential to effectively deliver health education and improve health behaviors among at-risk populations. To be successful, apps should include user input during stages of development. Previously, a prototype app designed for participants in the Texas Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) was developed based on input from focus groups.
Aims: This research aimed to continue app design by soliciting user input via a survey from a state-wide sample.
Methods: Texas WIC clients were asked about physical activity, healthy eating, and breastfeeding behaviors, stage of change regarding health behaviors, current use of health-related apps, and perceptions of app prototype features. Latent class analysis (n=942) was used to identify mutually exclusive groups based on the strength of participants’ agreement that prototype features would help them exercise more or consume more fruits and vegetables. Logistic regression examined health-related characteristics and sociodemographic differences between classes.
Results: Response to app prototype features was positive. A 2-class model best described latent classes. Class members that strongly agreed that prototype features would help them improve health behaviors were younger (< 35 years), not pregnant, already using health-related apps, and in the contemplation, preparation, or action stages of change regarding physical activity.
Conclusion: Refinement of the Texas WIC app should incorporate input from individuals who are pregnant, older than 35 years, or in pre-contemplation regarding physical activity. The iterative process of user-centered design applied in this research may serve as a useful framework for development of other public health apps.
Keywords: health promotion, technology, vegetables, smartphone, exercise
Introduction
In the United States, poverty affects women and children disproportionately, as they make up approximately 70% of the low-income population.1 Poverty is associated with deleterious health behaviors, such as consuming a low-quality diet and being physically inactive, particularly among vulnerable populations such as women and children.2 These behaviors contribute to serious health concerns, including poor birth outcomes, obesity, heart disease, type 2 diabetes, and certain cancers.2,3 Limited access to evidence-based information related to health, physical activity, nutrition, and infant care is a likely contributor to poor health behaviors and outcomes among low-income individuals and may be an important barrier that contributes to ongoing health disparities.2
Launched in 1972, the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is a federal grant program that serves low-income pregnant, postpartum, and breastfeeding women, infants, and children up to age 5 who are at nutritional risk, with the goal of improving health behaviors and outcomes during critical periods of development.4 Annually, 8 million women, infants, and children are enrolled in WIC, with approximately 886 thousand participating in the state of Texas.5 WIC provides a number of resources, including vouchers for healthful foods to support pregnancy, lactation, and growth, and referrals to health care services.6 While they are enrolled in the program, WIC clients are expected to regularly participate in education that focuses on promoting healthy behaviors such as breastfeeding, exercise, and healthy eating (e.g. eating fruits and vegetables, cooking meals at home, eating meals as a family).6 Historically, WIC clinics have worked to impart evidence-based information related to health behaviors through education offered at clinics via face-to-face education. This education modality presents barriers to an already taxed population, which may lack reliable transportation to clinics and childcare during education sessions.7 In an attempt to mitigate these barriers, many WIC state agencies now offer online client education.8 However, reliable access to a computer with internet connectivity is not ubiquitous among Americans, and low-income smartphone owners are more likely to rely on their smartphones as a primary way of connecting to the internet.9 Indeed, Texas WIC clients have expressed a desire to receive education and services delivered via phone.7,10 Thus, smartphone apps may offer a viable alternative interface for providing innovative, accessible, and customizable health education to the WIC population. Research has supported the use of smartphones as a behavioral modification tool, with a number of applications developed to improve diet and physical activity.11
Smartphone apps have unique characteristics that may make them particularly ideal for delivering health education and supporting health behavior change. For example, smartphone apps can be used to access clients in real time, offer continual assessment of identified treatment goals, and deliver meaningful information and support to reinforce behavior change.11 Despite the promise of smartphone apps, individuals tend to discontinue app use after three months of downloading.12 Therefore, app developers should consider, a priori, the expressed needs of intended users. Indeed, all approaches to developing technological tools to improve health outcomes should engage people first.13 One approach to developing apps that prioritizes individuals is user-centered design (UCD), an evidence-based, iterative process prioritizing user input and engagement in designing products and services.14 Because UCD has been previously used to develop appealing smartphone apps that target health behaviors, such as physical activity,15 this process shows promise for developing an effective app for WIC clients. In 2014, based on strong interest among Texas WIC clients for delivery of nutrition education and services via their smartphones,16 the Texas Department of State Health Services WIC program commissioned us to develop a smartphone app prototype. To do this, we began the UCD process by conducting focus groups with a diverse sample of female WIC participants in south central Texas to explore current smartphone app use and preferences.17 Based on this initial user-input and tenets of the Social Cognitive Theory,18 we developed an app prototype, designed to provide customizable, interactive, and user-centered health education to the Texas WIC population.17 The prototype included features to support physical activity (i.e., activity calendar, activity tracker, exercise videos, resource library), healthy eating (i.e., meal calendar, healthy eating tracker, cooking videos, resource library, shopping list, fruit and vegetable game, farmer’s market locator), and breastfeeding (i.e., breastfeeding timer, growth chart, live assistant, resource library).17
The aim of this research was to continue the UCD process of developing an app for Texas WIC clients by disseminating a statewide survey seeking input regarding the app prototype features. Analysis of clients’ perceptions of prototype features designed to support physical activity and healthy eating are included in this report. Our approach was to use latent class analysis to identify subgroups of respondents based on the extent to which they agreed that the features would help them increase physical activity and intake of fruits and vegetables, and logistic regression to examine how membership in the latent classes were associated with sociodemographic and health-related characteristics. Recommendations for continued user-centered design of the WIC app were informed by characteristics of respondents in latent classes.
Methods
Sample
The survey was posted on the Texas WIC website from September 9, 2014 through November 6, 2014. Clients visiting the website were greeted with a pop-up window presenting an offer to take the survey in English or Spanish. Additionally, clinics in central Texas who had access to client email addresses sent invitations to clients to take the survey. Of the 606 emails sent, 88 addresses were invalid, 102 began taking the survey, and 63 finished. Overall, 1,019 WIC clients completed the survey. Participants who were younger than 18 (n=50), male (n=14), and had an implausible reported height (shorter than 4 feet or taller than 7 feet, n=27)19 were removed from the analytic sample, leaving a total sample of 942 respondents. The Institutional Review Boards of Texas State University and the Texas Department of State Health Services approved this study.
Survey
The survey, developed in English in collaboration with Texas WIC staff, included approximately 130 questions, depending on responses to logic-driven branches. To develop a version of the client survey in Spanish, the English survey was translated to Spanish, back-translated, and discrepancies were reconciled. The survey was implemented using Qualtrics software (2014, Provo, UT). The welcome page briefly described the survey, provided assurances of privacy, and described incentives for survey completion, which included credit for taking a WIC nutrition class and receiving a t-shirt. After giving informed consent, participants were asked if they owned a smartphone. Those who responded with ‘no’ were routed to a thank you page and the survey was discontinued.
The survey was divided into 3 major sections corresponding to health behaviors addressed by the WIC app prototype, including physical activity, healthy eating, and breastfeeding, followed by a set of demographics questions. Each health behavior section asked about current health practices, stage of change, facilitators and barriers to performing the health behavior, belief that app features would help to improve health behaviors, and current use of apps regarding that health behavior. Facilitators and barriers to health behaviors were drawn from focus groups held during the initial phase of the UCD of this prototype app.17 The current study is an analysis of participant response to the physical activity and healthy eating features and does not include breastfeeding.
Current practices regarding physical activity were measured using the Godin leisure-time exercise questionnaire, which creates a physical activity score based on questions about intensity and duration of exercise.20 This score classifies participant activity as insufficiently active, moderately active, or active. For analysis, categories were collapsed into a binary variable (0 = insufficient activity, 1 = moderately active or active). Stage of change for physical activity behaviors was assessed using a 4-question system adapted from Wolf et al. (1 = pre-contemplation, 2 = contemplation, 3 = preparation, 4 = action).21 Survey respondents were asked to indicate on a 5-item Likert scale to what extent they agreed that specific barriers and facilitators to physical activity applied to them personally (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree); these data were not included in this analysis. Finally, after each of the four app prototype features addressing exercise was displayed (an activity calendar, activity tracker, exercise videos, and resource library), clients were asked whether they agreed that the feature would help them exercise more often (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree).
Intake of fruits and vegetables was used as an indicator of healthy eating practices and was measured using a brief screener employed by Wolf et al. (fruit and vegetable servings consumed on the previous day, excluding servings of white potatoes, were summed for the final count and included in analysis as a continuous variable).21 Participants were also asked how many family meals they had each week, which was included as a continuous variable. Assessments of stage of change and whether the seven prototype features (a meal calendar, healthy eating tracker, cooking videos, a resource library, shopping list, fruit and vegetable game, and a farmer’s market locator) that addressed healthy eating would help them eat more fruits and vegetables were conducted in the same manner as described for physical activity.
The survey included questions about demographic characteristics. Household size was measured as a continuous variable. Age of participants (0 = 35 years or older, 1 = younger than 35 years), education (0 = high school or less, 1 = post-secondary education), race/ethnicity (White = reference, Black, Hispanic, Other), language used to complete the survey (0 = English, 1 = Spanish), employment status (0 = unemployed, 1 = employed), location of residence (0 = urban, 1 = rural), and body mass index (BMI; < 18.5 = underweight, 18.5 – 24.9 = normal weight, 25 – 29.9 = overweight, > 30 = obese) were coded as categorical variables. Due to few participants having a BMI identifying them as underweight, participants identified as underweight and normal weight were combined and used as the BMI reference group. BMI was not calculated for women who were pregnant (1 = pregnant, 0 = not pregnant). Food security was assessed with the U.S. Household Food Security Survey Module: Six-Item Short Form.22 Food security status was coded as a dichotomous variable (0 = very low or low food security, 1 = marginal or high food security). Current use of physical activity or healthy eating apps were coded as dichotomous variables (0 = never or almost never use, 1 = sometimes or daily use).
Statistical analyses
Latent class analysis, a form of mixture modeling allowing for the classification of unobserved heterogeneity in responses to multiple variables, was used to identify homogenous, mutually exclusive groups of WIC clients based on the extent to which they agreed that prototype features would help them exercise more often or eat more fruits and vegetables.23 To identify the number of classes that best represented the underlying response groups, a series of model fit tests were conducted starting with a single-class model. Model fit indices, including Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and sample-size adjusted AIC (SSA-AIC), were used to determine whether the inclusion of each additional class provided improved model fit. Model entropy, representing the accuracy of assigning individuals to classes, was also considered. Finally, the Vuong-Lo-Mendell-Ruben (VLMR) likelihood ratio provided a statistical test of whether the estimated model significantly improved model fit compared to a model with one less class. Once the optimal number of latent classes was determined, logistic regression was used to examine differences between classes based on sociodemographic and health-related characteristics. The latent class analysis and logistic regression was conducted with Mplus 7.324 using maximum likelihood estimation with robust standard errors, providing treatment of missing data with maximum likelihood and estimation of standard errors robust to non-normality. All other analyses were conducted using IBM SPSS Statistics for Windows, version 24 (IBM Corp., Armonk, N.Y., USA).
Results
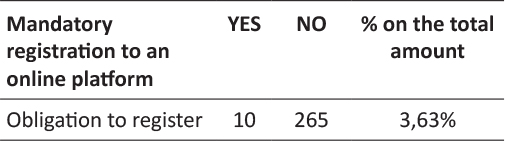
Table 1 presents model fit indices used to identify the optimal number of latent classes based on WIC participants’ responses to the survey questions “this app feature would help me exercise more/eat more fruits and vegetables.” Compared to the 1-class model, the 2-class model had improved AIC, BIC, and SSA-BIC model fit indices; the rate of model fit improvement decreased with the 3-class model. The VLMR test indicated that the 2-class model was a significant improvement on the 1-class model (p < .001), but the 3-class model was not a significantly better fit than the 2-class model (p = 0.8). Thus, based on model fit tests and the necessity of parsimony, the 2-class model was identified as the best description of latent classes.
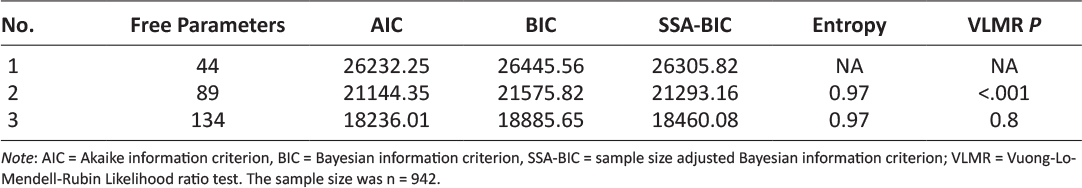
Table 1: Goodness of fit indices for determining number of latent classes among Texas WIC survey respondents.
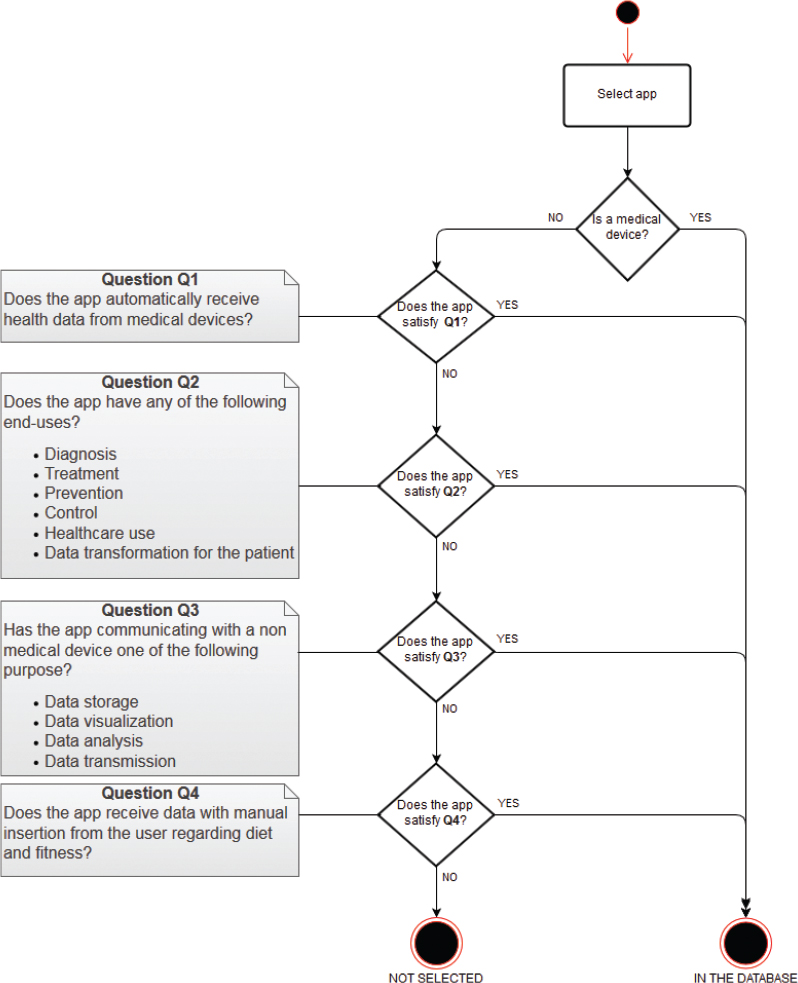
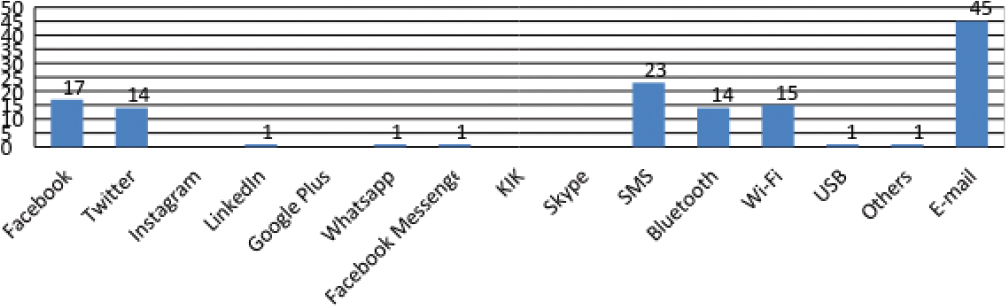
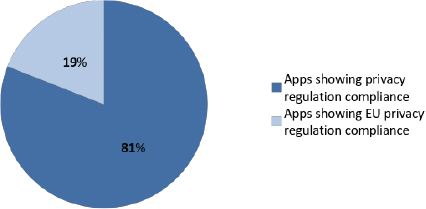
Class 1 (strongly agree; 32.9% of the sample) was identified as the group that strongly agreed that app features would help them improve targeted health behaviors; those in class 2 (neutral, agree; 64.8% of the sample) agreed or were neutral regarding whether the app features would help improve health behaviors. Figure 1 shows the distribution of responses to questions asking if using the app features would help respondents improve targeted health behaviors.
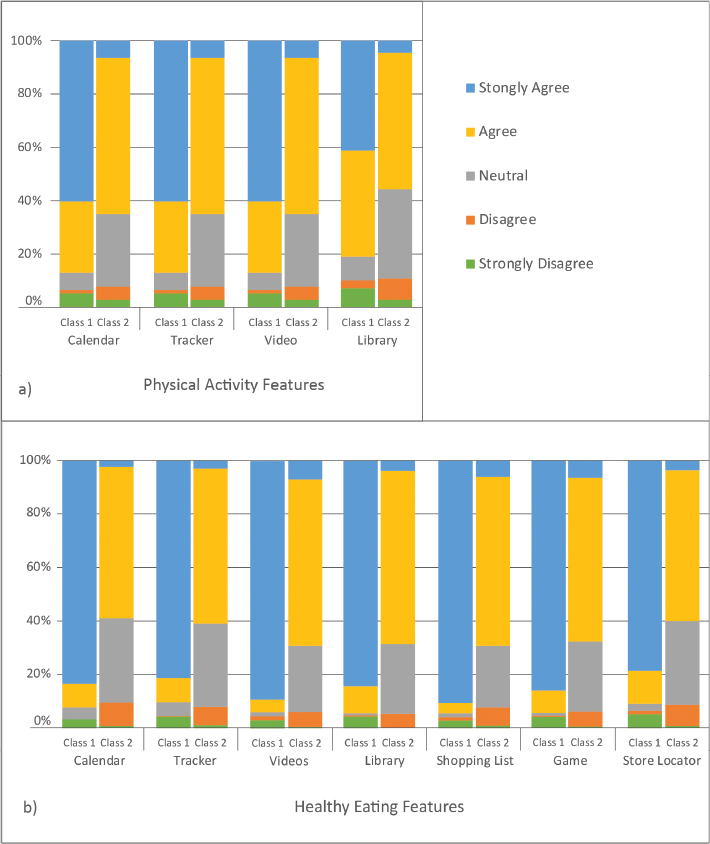
Figure 1: WIC clients’ agreement that app features would help improve targeted health behaviors. a) Depicts Class 1 (strongly agree) and Class 2 (neutral, agree) feedback regarding physical activity features. b) Depicts Class 1 (strongly agree) and Class 2 (neutral, agree) feedback regarding healthy eating features.
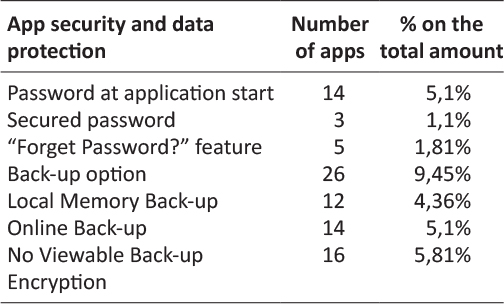
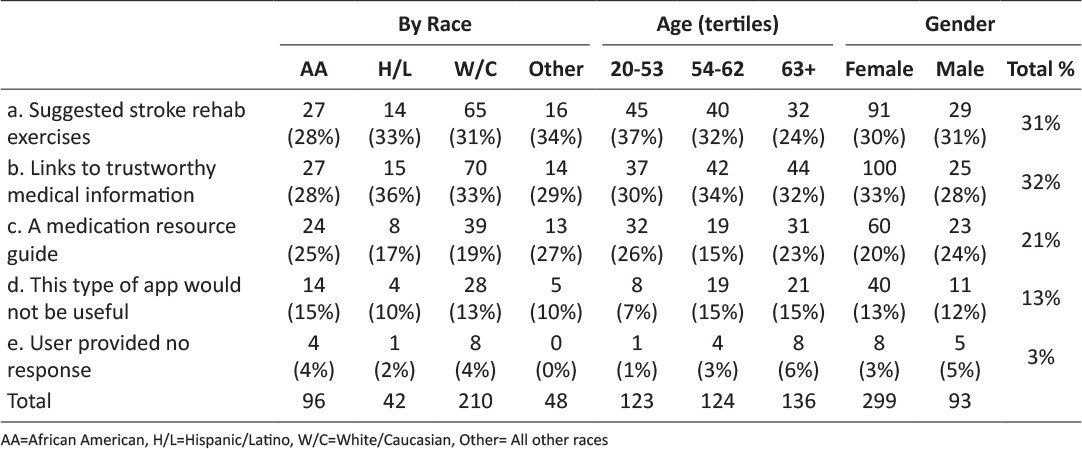
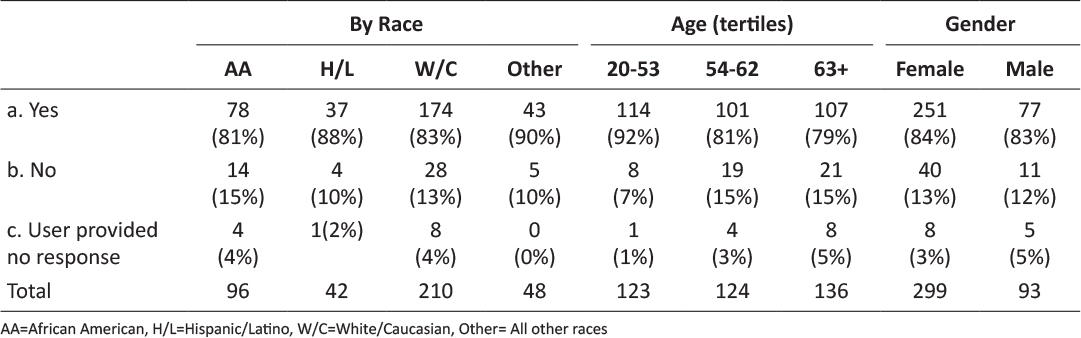
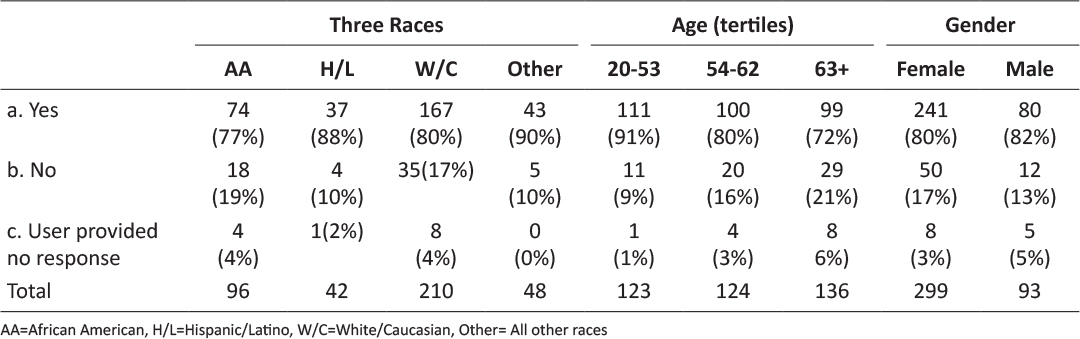
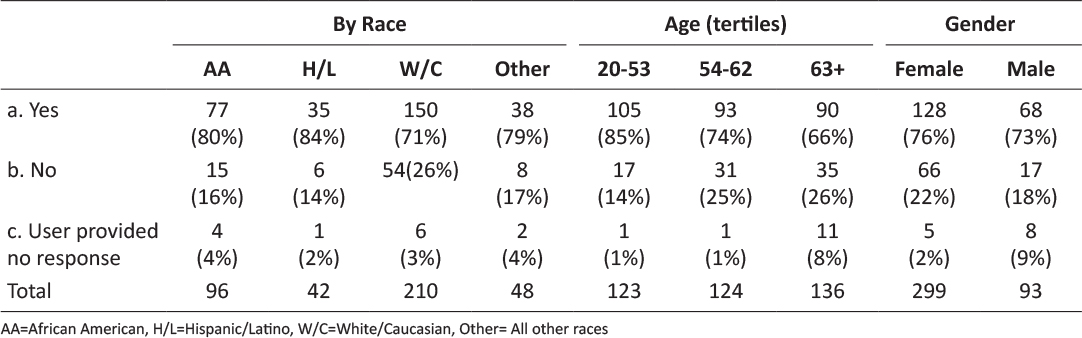
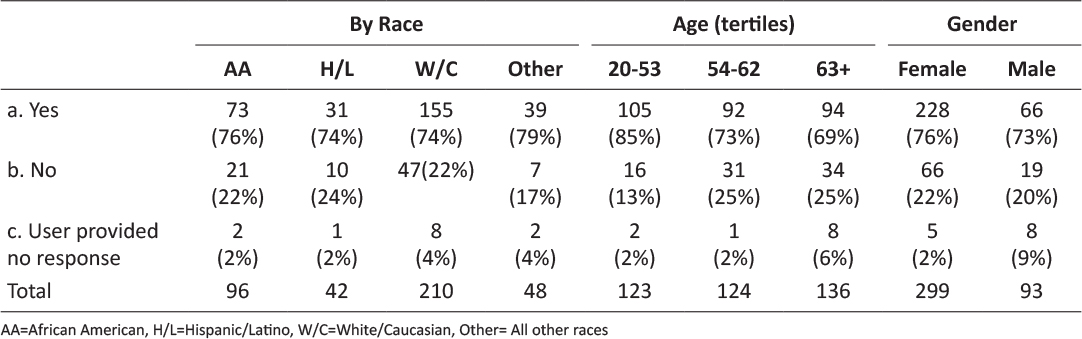
Table 2 includes descriptive statistics for the complete analytic sample as well as by latent class. On average, respondents in the complete sample had approximately 5 household members and consumed 7.4 family meals per week, including 3.5 servings of fruits and vegetables per day. Approximately three out of four respondents were younger than 35 years of age at the time of the survey, which categorizes them as millenials.25 Slightly more than half of participants were Hispanic and the vast majority took the survey in English. Approximately 45% of respondents were employed and the majority were urban-dwellers. Fifty-eight percent were overweight or obese. Sixteen percent of the sample was pregnant. Approximately a third of the sample had completed post-secondary education and a third had marginal or high food security. Two-thirds engaged in at least 150 minutes of moderate or intense physical activity each week. Almost two-thirds of participants used apps for exercise and three-quarters used healthy eating apps. The vast majority recognized the benefits of being physically active and eating fruits and vegetables. Likewise, the majority were in contemplation, preparation, or active stages of change regarding being physically active and eating fruits and vegetables.
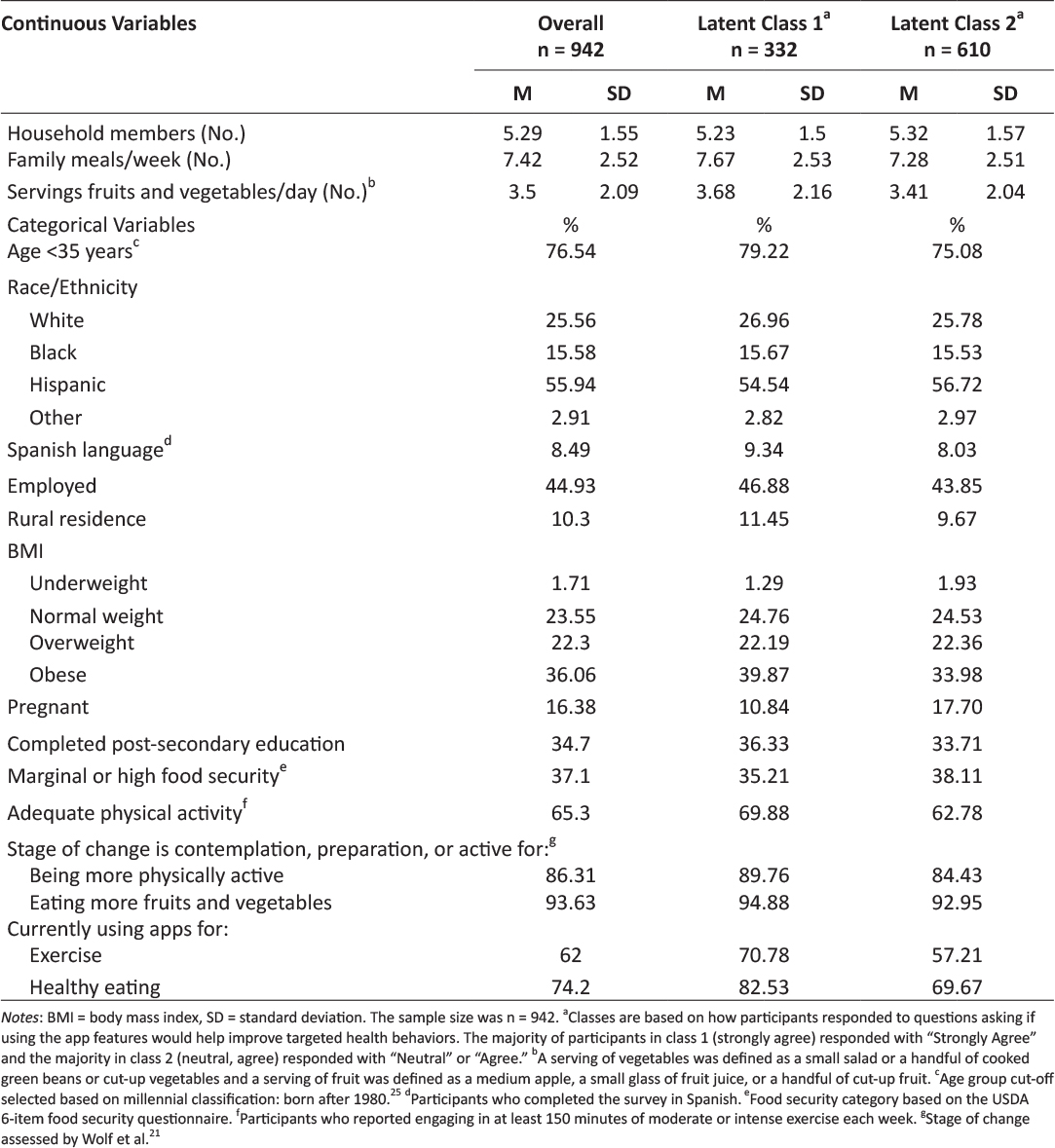
Table 2: Description of the overall sample of Texas WIC clients and the 2 latent classes.
The results of the multinomial logistic regression are shown in Table 3; class 2 (neutral, agree) was used as the reference group. Age, pregnancy, current app use, and stage of change regarding exercise were significant predictors of class membership. Specifically, respondents were more likely to be in class 1 (strongly agree) if they were younger than 35 years old (OR = 1.40; CI = 1.05, 1.86), were in contemplation, preparation, or active stages of change regarding exercise (OR = 2.28, CI = 1.26, 4.11), or were currently using apps for exercise (OR = 1.33; CI = 1.02, 1.78) or healthy eating (OR = 1.72, CI = 1.22, 2.42). Respondents were significantly less likely to be in class 1 (strongly agree) if they were pregnant (OR = 0.55, CI = 0.37, 0.82).
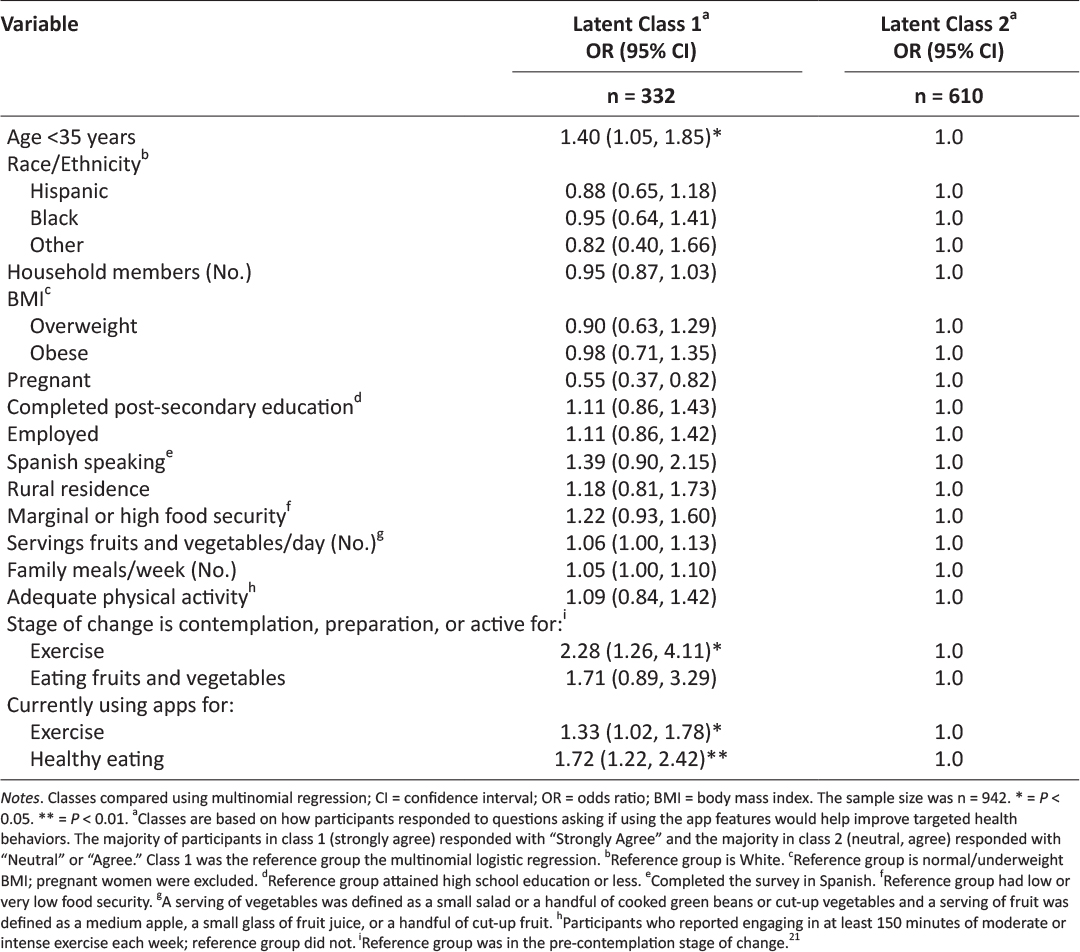
Table 3: Predictors of Texas WIC clients’ perceptions of WIC app prototype features.
Discussion
This paper describes an intermediate stage of UCD of an app designed for Texas WIC participants. By investigating variation in responses to the app prototype features, our aim was to identify characteristics of survey respondents associated with the strength of their agreement that the physical activity and healthy eating features would help them improve targeted health behaviors. Importantly, survey respondents’ reactions to the app prototype features were positive. Participants who strongly agreed that the app features would help support behavior changes were more likely to be younger than 35 years of age, in the contemplation, preparation, or action stages of change for the targeted health behaviors, and currently using apps to foster these health behaviors.
The influence of age on class membership is not unexpected. Indeed, millennials, or those born after 1980, are the age group most likely to be continually engaged with smartphones26 and use them for a variety of activities such as searching for jobs and accessing health information.27 One potential avenue for increasing the acceptability of this app among older WIC participants would be to link to or otherwise leverage platforms that have cross-generational appeal.28 In the context of the transtheoretical model, it is also not surprising that participants in contemplation, preparation, or action stages of change were more likely to view the proposed app features as supportive, as they were already interested in improving the targeted health behaviors.29 Similarly, individuals currently using apps are likely more receptive to prototype app features, in general. A surprising finding was that pregnancy was a significant predictor of class membership, with pregnant women being half as likely to be in class 1 (strongly agree). Previous research has reported that, in general, pregnant women are interested in health-related apps with features that are provide information specific to pregnancy, such as pregnancy-related risk factors, gestational weight gain, diet and lifestyle, postpartum depression, social support, and early infant feeding.30–32 In light of this, one explanation for the relatively tepid response of pregnant women in this study could be that the features were not specific to dietary and exercise recommendations for pregnancy. Additionally, mobile health interventions targeting pregnant women often suffer from low enrollment and high attrition, suggesting that, in general, pregnancy may be a challenging time to address health behavior change.33 However, firm conclusions about the allure of mobile apps to address health behaviors during pregnancy cannot be drawn due to a dearth of relevant studies.33 Given that health behaviors during pregnancy can have a profound impact on maternal and child health, it is important for an app designed for WIC clients to specifically address the needs of pregnant women to support a healthful pregnancy.
A strength of this study was the use of a large sample of Texas WIC clients who have experience with technology. Sample demographics were somewhat comparable to Texas WIC, with 56% of the sample being Hispanic, compared to 68% in Texas WIC,34 and 58% being overweight or obese, compared to 52% in Texas WIC.35 Limitations include electronic recruitment of individuals who owned a smartphone, resulting in a sample biased towards technology use.
Conclusion
Given the enthusiastic response to the Texas WIC app prototype, it would be tempting to finalize app development by simply incorporating the features described in this study. However, while many factors may impact the ultimate success of public health apps, perhaps a central piece revolves around the needs and preferences of the intended user, framed within the context of his or her specific life’s challenges.13 A user-centered approach to developing technology-based tools, such as the UCD process, is a critical step in ensuring that public health interventions reach their target audiences and elicit desired health outcomes.14 Given the health status of vulnerable populations, such as low income women and children participating in WIC,2 developing and implementing efficacious, evidence-based, population-specific tools and technologies that meet the needs of participants is of paramount importance, and may provide a catalyst to improve health equity by removing barriers to accessing information. In the case of the development of a Texas WIC app, engaging clients who are older, in a pre-contemplation stage of change, or pregnant should occur next, so that their specific needs and preferences can be incorporated into the final version. The iterative process of UCD used in this research may serve as a useful framework for development of public health apps.
Acknowledgements
This research was funded by a grant from the Texas Department of State Health Services (contract number 2014-045584). WIC staff provided input on prototype feature design,17 reviewed survey content, and facilitated survey dissemination via their website.
Disclosures
The Institutional Review Boards of Texas State University (2013E3835) and the Texas Department of State Health Services (14-014) approved this study.
Declaration of Competing Interests
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: all authors had financial support from the Texas Department of State Health Services for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
References
1. Legal Momentum. Women and Poverty in America. Available from: https://www.legalmomentum.org/women-and-poverty-america. Accessed December 2016.
2. Adler NE, Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Ann N Y Acad Sci. 2010;1186:5-23. ![]()
3. Eidelman AI, Schanler RJ, Johnston M, et al. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827-e841. ![]()
4. Oliveira V, Racine E, Olmsted J, Ghelfi LM. The WIC Program: Background, trends and issues (No. 33847). United States Department of Agriculture, Economic Research Service; 2002.
5. United States Department of Agriculture Food and Nutrition Service. WIC Program: Total Participation. Available from: https://www.fns.usda.gov/sites/default/files/pd/26wifypart.pdf. Accessed July 2017.
6. Special Supplemental Nutrition Program for Women, Infants, and Children. 7 C.F.R. §246.11 1985. Available from: http://www.ecfr.gov/cgi-bin/text-idx?SID=a42889f84f99d56ec18d77c9b463c613&node=7:4.1.1.1.10&rgn=div5#se7.4.246_111. Accessed July 2017.
7. Greenblatt Y, Gomez S, Alleman G, et al. Optimizing nutrition education in WIC: Findings from focus groups with Arizona clients and staff. J Nutr Educ Behav. 2016;48(4):289-294. ![]()
8. Cates S, Capogrossi K, Sallack L. WIC Nutrition Education Study: Phase I Report. Alexandria, VA: United States Department of Agriculture, Food and Nutrition Service, Office of Policy Support; 2016. Available from: https://fns-prod.azureedge.net/sites/default/files/ops/WICNutEd-PhaseI.pdf. Accessed June 2017.
9. McHenry G. Evolving technologies change the nature of Internet use. National Telecommunications and Information Administration. Available from: https://www.ntia.doc.gov/blog/2016/evolving-technologies-change-nature-internet-use. Accessed July 2017.
10. Deehy K, Hoger FS, Kallio J, et al. Participant-centered education: Building a new WIC nutrition education model. J Nutr Educ Behav. 2010;42(3S):S39-S46. ![]()
11. Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: A systematic review. Int J Behav Nutr Phys Act. 2016;13(1):127. ![]()
12. Localytics. Helping marketers better understand app user trends. Available from: http://www.localytics.com/resources/app-stickiness-index-q1-2015. Accessed July 2017.
13. Barclay G, Sabina A, Graham G. Population health and technology: Placing people first. Am J Public Health. 2014;104(12):2246-2247. ![]()
14. McCurdie T, Taneva S, Casselman M, et al. mHealth Consumer apps: The case for user-centered design. Biomed Instrum Technol Mob Heal. 2012;Suppl:49-56. ![]()
15. Vorrink SN, Kort HS, Troosters T, et al. A mobile phone app to stimulate daily physical activity in patients with chronic obstructive pulmonary disease: Development, feasibility, and pilot studies. JMIR mHealth uHealth. 2016;4(1):e11. ![]()
16. Texas WIC Nutrition Education Survey – Statewide Report. Texas Department of State Health Services; 2016. Available from: https://www.dshs.texas.gov/wichd/bf/surveysreports.aspx. Accessed July 2017.
17. Biediger-Friedman L, Crixell SH, Silva M, et al. User-centered design of a Texas WIC app: A focus group investigation. Am J Health Behav. 2016;40(4):461-71. ![]()
18. Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Adv Behav Res Ther. 1978;1(4):139-161. ![]()
19. Koebnick C, Smith N, Huang K, et al. The prevalence of obesity and obesity-related health conditions in a large multiethnic cohort of young adults in California. Ann Epidemiol. 2012;22(9):609-616. ![]()
20. Godin G, Shephard R. Godin leisure-time exercise questionnaire. Med Sci Sport Exerc. 1997;29(6):S36-S38.
21. Wolf RL, Lepore SJ, Vandergrift JL, et al. Knowledge, barriers, and stage of change as correlates of fruit and vegetable consumption among urban and mostly immigrant black men. J Am Diet Assoc. 2008;108(8):1315-1322. ![]()
22. United States Department of Agriculture Economic Research Service. Household Food Security Survey Module: Six-Item Short Form. Available from: https://www.ers.usda.gov/media/8282/short2012.pdf. Accessed May 2014.
23. Hagenaars J, McCutcheon A, eds. Applied Latent Class Analysis. Cambridge, UK: Cambridge University Press; 2002. ![]()
24. Muthén L, Muthén B. Mplus User’s Guide. Vol 7th ed. Los Angeles, CA: Muthén & Muthén; 2015.
25. Experian. Millennials and Technology: The Natural Order of Things. Available from: http://www.experian.com/blogs/marketing-forward/2014/07/07/millennials-and-technology-the-natural-order-of-things. Accessed July 6, 2017.
26. Nielsen. Millennials are Top Smartphone Users. Available from: http://www.nielsen.com/us/en/insights/news/2016/millennials-are-top-smartphone-users.html. Accessed July 2017.
27. Pew Research Center. U.S. Smartphone Use in 2015. Available from: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/. Accessed June 2015.
28. Pew Research Center. Social Media Update 2016. Available from: http://www.pewinternet.org/2016/11/11/social-media-update-2016/. Accessed May 2018.
29. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Heal Promot. 1997;12(1).
30. Osma J, Barrera AZ, Ramphos E. Are pregnant and postpartum women interested in health-related apps? Implications for the prevention of perinatal depression. Cyberpsychology, Behav Soc Netw. 2016;19(6):412-415. ![]()
31. Krishnamurti T, Davis A, Wong-Parodi G, et al. Development and testing of the MyHealthyPregnancy App: A behavioral decision research-based tool for assessing and communicating pregnancy risk. JMIR Mhealth Uhealth. 2017;5(4):e42. ![]()
32. Waring ME, Moore Simas TA, Xiao RS, et al. Pregnant women’s interest in a website or mobile application for healthy gestational weight gain. Sex Reprod Healthc. 2014;5(4):182-184. ![]()
33. O’Brien CM, Cramp C, Dodd JM. Delivery of dietary and lifestyle interventions in pregnancy: Is it time to promote the use of electronic and mobile health technologies? Semin Reprod Med. 2016;34(2):e22-e27. ![]()
34. United States Department of Agriculture Food and Nutrition Services. WIC Racial-Ethnic Group Enrollment Data 2012. Available from: https://www.fns.usda.gov/wic/wic-racial-ethnic-group-enrollment-data-2012. Accessed July 2017.
35. Johnson B, Thorn B, McGill B, et al. WIC Participant and Program Characteristics 2012. Alexandria, VA: United States Department of Agriculture, Food and Nutrition Service; 2013. Available at https://www.fns.usda.gov/wic/women-infants-and-children-wic-participant-and-program-characteristics-2012. Accessed June 2017.
Read More