Nicole Koehler1, Olga Vujovic2, Christine McMenamin1
1Assesment and Learning Design, Deakin Learning Futures, Deakin University, Burwood Campus, Australia 2Department of Infectious Diseases, Alfred Hospital, Victoria,Australia 3Faculty of Medicine, Nursing & Health Sciences, Monash University, Victoria, Australia
Corresponding Author: nicole.koehler@deakin.edu.au
Journal MTM 2:1:14-21 2013
DOI:10.7309/jmtm.2.1.3
Background: New technology such as the internet and mobile phone applications (“apps”) are increasingly being used in clinical practice. However, little is known in regards to individual’s attitudes towards medical professionals using the internet and apps in the context of their own medical care. The aim of the present study was to examine and compare individual’s attitudes towards the use of medically related internet sites and apps in clinical practice.
Method: Participants completed an on-line survey which contained questions regarding their own use of mobile phones and the internet, their use of healthcare facilities, and their attitudes towards medical professionals using the internet and apps during consultations. Attitudes were assessed by asking participants to rate 11 statements on a 5 point scale.
Results: The survey was completed by 141 individuals. All participants owned a mobile phone, with 82% owning one with application support. Furthermore, all participants had access to the internet at home. Generally participants had more favourable attitudes towards medical professionals using the internet than apps. For example, participants found it more acceptable for doctors to use medically related internet sites than mobile phone apps during consultations with patients.
Conclusion: It is possible that attitudes towards the internet were more favourable than that for apps because the internet has been available longer and consequently individuals are more familiar with it. Prior to using newer electronic resources, especially apps, medical professionals should adequately inform patients in regards to their intended use to avoid potential misconceptions.
Introduction
The end of the last century saw the introduction of the internet which was rapidly taken up by the general public such that 79% of individuals living within Australia accessed the internet at home by 2010-111. At the start of this century smartphones (e.g., iPhone and Blackberry), which combine the conventional functions of a mobile phone with advanced computing capabilities2-3, were publically launched. Smartphones are also capable of supporting applications, commonly termed “apps”, and consequently with an increase in smartphone use, app use also increased2. The use of technology such as the internet and apps also made their way into the medical profession4. Currently there are more than 10,000 apps within the Apple App Store’s “medical, health care & fitness” category5. These apps, many of which have been specifically designed to assist medical professionals and medical students, include but are not limited to medical calculators4-6, logbooks4, medical reference tools7, clinical guidelines such as resuscitation algorithms4 and drug guidelines6.
Given the abundance of medical apps currently available it is crucial that their efficacy is rigorously evaluated before implementing their use8. More specifically, it is vital to ensure that the use of an app does not delay the onset of patients’ receiving medical care, especially when timing is critical (e.g., assessment of an ischemic stroke or initiating cardiopulmonary resuscitation), and ultimately that the use of an app actually improves the patient’s outcome8-11. Several studies have evaluated the use of apps, some of which we will briefly reviewed here.
Josephson and Salman evaluated the use of a specifically designed app to assess and manage an ischemic stroke9. They found that healthcare professionals’ performance was 20 seconds longer when using the app compared to when using the traditional paper based method. However, caution must be taken when drawing conclusions from this study because it was based on three participants and a lack of familiarity with using an app may have contributed to participants’ performance. In another study, Zanner and colleagues evaluated the general public’s use of a specifically designed cardiopulmonary resuscitation app in a hypothetical emergency scenario in regards to participants’ accuracy of performance (i.e., tasks performed correctly) and speed of performance11. Participants who used the app performed significantly slower than those in the control group, but received higher accuracy of performance scores although this difference was not statistically significant11. Overall, using the app did not improve patient outcome. Once again, a lack of familiarity with the app, despite having predominantly final year school students who are familiar with mobile phones making up their participant group, could have contributed to participants’ performance11. On the other hand, a study involving doctors, with advanced life support training, found that those given a specifically designed resuscitation app scored significantly better in regards to their resuscitation performance in a simulated situation compared to those without the app10. Another study concerning the accuracy of performing a task found that 100% of participants (doctors and medical students) who used a specifically designed app to calculate drug infusions were correct in regards to their calculation whereas only 28.6% of them were correct when using the traditional printed guide. Furthermore, participants were faster and more confident in their calculation when they used the app compared to using the traditional method12. Perhaps this finding can be partially attributed to the younger generations’ dependency on calculators in terms of performing arithmetic tasks. These mixed results regarding the efficacy of apps clearly show that apps may be suitable for some tasks more so than others and thus critically evaluating apps prior to implementation is essential.
Not only have medical apps been used in clinical practice, and developed for use by the general public in emergency situations, but they have also made their way into medical education. We recently surveyed medical students in regards to their use of medical apps and found that 72% of medical students already use them13. Furthermore, 94% of students who have a smartphone without medical apps are considering obtaining them and 72% of medical students without a smartphone were considering obtaining one so that they can access medical apps13. These results suggest that the use of medical apps in clinical practice is likely to increase in the future given the high prevalence of medical app use amongst current medical students in addition to many students intending to obtain them. However, despite many medical students already using medical apps, it was interesting to note that several students expressed concerns regarding the use of apps in clinical practice within the free written comments section at the end of the survey. Several students felt that patients would feel that they are using their smartphones for non-medical related purposes such as accessing social media sites or texting friends – e.g., “I feel it’s inappropriate to use iPhones infront [sic] of patients / other clinicians because they assume you are smsing or something not relevant”. Whereas others simply felt that patients would perceive them to be rude if they used their smartphone because they are not familiar with such technology – e.g., “I think it looks unprofessional when Drs and students are using their phones all the time, regardless of the purpose. Many older patients are unfamiliar with the technology and I think they would find it rude.” These comments have prompted us to explore whether students’ perceptions in regards to patients’ attitudes towards smartphone use are in fact true.
To the best of our knowledge little is known in regards to the individual’s attitudes towards medical professionals using medical apps within clinical practice. Thus the aim of our study was to evaluate the individual’s attitudes towards the use of smartphones (and apps) in clinical practice. Additionally, our study also evaluated individuals’ attitudes towards use of the internet in clinical practice, providing a comparison measure because the internet has been available longer than smartphones and thus individuals are likely to be more familiar with it. Thus, given the higher level of familiarity with the internet, it is hypothesised that individuals will have more favourable attitudes towards the use of the internet than smartphones in clinical practice.
Furthermore, given that both financial and medical information have some element of confidentiality associated with it we specifically asked participants whether they use the internet and/or smartphone to conduct on-line banking. Questions pertaining to on-line banking were asked to determine whether individuals who do not conduct on-line banking have greater concerns in regards to medical professionals using the internet and smartphones than those that conduct on-line banking. We acknowledge that financial and medical data are not analogous but we believe that it is the best comparison in terms of privacy that is currently available.
Research Methodology
Participants
Staff and students at Monash University were invited to participate in an on-line survey on their attitudes towards the use of smartphones (and apps) and the internet in clinical practice via an advertisement on Monash Notices (a weekly electronic university newsletter). Additionally, upon survey completion, participants were offered the opportunity to forward the survey link to family and friends. Individuals aged 18 years and over were eligible to participate.
Procedure
Ethics approval for the study was obtained from the Monash University Human Research Ethics Committee. Participants were directed to the on-line survey via a link contained within the recruitment advertisement. Participation was anonymous and voluntary. No reimbursement was offered to participants.
The first two sections of the survey obtained participants’ demographics and information pertaining to their mobile phone ownership and app use. A definition of the term “mobile phone application” was provided together with an example of an app in case participants were unfamiliar with the concept. The third section ascertained participants’ internet access and use. Within the fourth section participants were asked in regards to their use of healthcare facilities and whether their medical practitioner used the internet and apps to obtain medical information in their presence.
The final two sections of the survey established participants’ attitudes towards the use of medically related internet sites and apps in clinical practice. Participants were instructed to rate eleven statements pertaining to internet use within clinical practice on a 5 point scale (1 = strongly disagree, 5 = strongly agree). The section pertaining to apps was analogous to the section on the internet in that the word “internet” was substituted for “mobile phone application” and when required the statements were altered slightly to make grammatical sense to accommodate the word substitution.
Results
One-hundred-and-forty-one participants (94 females) completed the survey of which 36 were Monash University students, eight were Monash University staff members and the remainder were not affiliated with Monash University. Participants had a mean age of 30.1 years (n = 141, SD = 12.9, range = 18-68). All, but five, participants resided within Australia. Thirty-six participants were either studying for or had obtained a medical/health professional qualification at the time of the survey.
Mobile phone and internet use
All participants owned a mobile phone and all, but one, participant owned a type of computer (e.g., desktop, laptop/notebook, tablet). All participants had access to the internet at home and with the exception of two participants accessed it at least once a day.
Most participants (82.3%) indicated that their mobile phone has app support (i.e., they had a smartphone) whereas the remaining participants indicated that they have a mobile phone without app support (13.5%) or that they did not know (4.3%). Ninety per cent of participants whohad a smartphone had apps and 84% of these participants used an app at least once a day. Thirty-one per cent of all participants were aware of medical apps (e.g., St John Ambulance Australia First Aid app).
In response to the statements “I find mobile phone applications useful in accessing information” and “I find the internet useful in accessing information”, 86% (n = 105) and 94% (n = 141) of participants respectively indicated that they either agreed or strongly agreed with this statement.
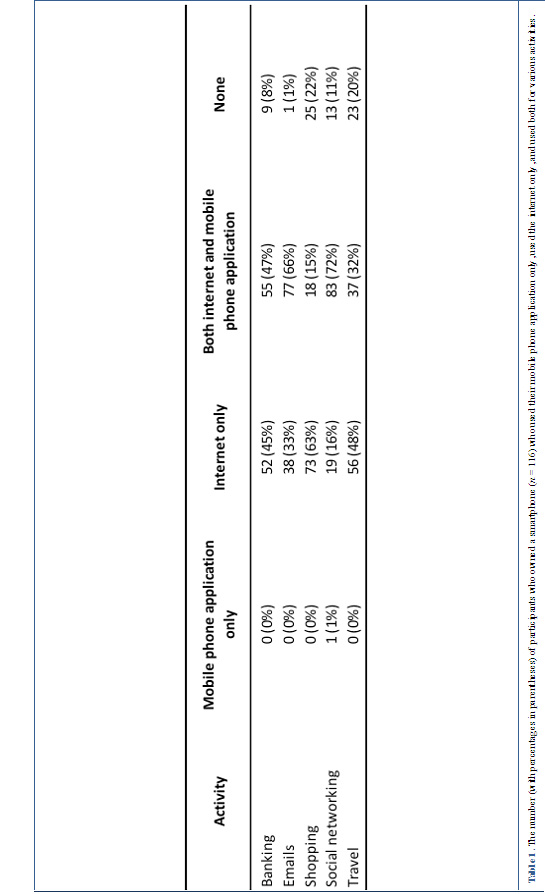
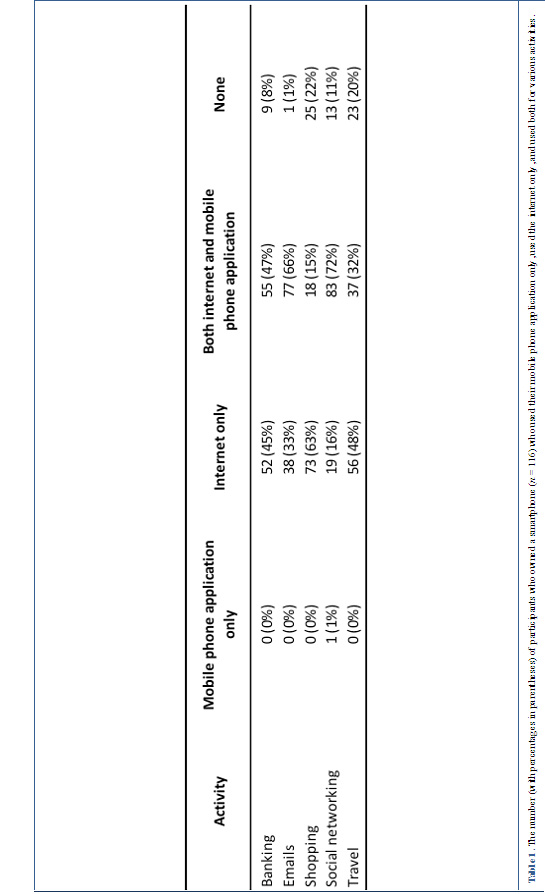
For participants who owned a smartphone, use of mobile phones and the internet for various activities was compared. As can be seen in table 1, all participants who used apps also used the internet for the following activities: banking, emails, shopping, and travel. Only one participant used apps, but not the internet, for social networking.
Healthcare facilities
All participants visited a healthcare facility at some point in their lives. Ten per cent did not visit a healthcare facility within the last 12 months. Only 14% of participants indicated that they have a medical condition that required regular visits to a healthcare facility.
Just over a third of participants indicated that a doctor accessed the internet in their presence to obtain medical information while treating them (39%), whereas the remaining participants indicated that this did not occur (29%) or they did not know (32%). On the other hand, only 1% of participants indicated that a doctor used an app in their presence, whereas 86% indicated that this did not occur and 13% did not know.
The majority of participants indicated that consultation notes were typed into their file on a desktop computer / laptop / notebook the last time they saw a doctor (74%). The remaining participants indicated that notes were handwritten in their file (21%), that notes were handwritten in their file and typed onto a computer (1%), that no notes were recorded in front of them (1%), and that they do not recall how notes were recorded (2%). None indicated the use of a smartphone to record notes.
Attitudes regarding the use of medically related internet sites and apps in clinical practice
Participants were asked to rate statements pertaining to the use of the internet and apps in clinical practice. Ratings were assigned a number between 1 and 5 (i.e., 1 = strongly disagree; 5 = strongly agree) and a mean rating was calculated for each statement. Paired sample t-tests were conducted for each pair of statements. As can be seen in table 2, participants had statistically significantly higher mean scores (i.e., indicating more agreement) for all positive statements pertaining to the internet than apps. Furthermore, with the exception of one statement, participants had statistically significantly lower mean scores (i.e., indicating more disagreement) for negative statements pertaining to the internet than apps. For the statement in regards to medical students relying excessively on the internet / apps there was no significant difference between participants’ mean ratings.
Participants who were studying towards or had obtained a medical/health professional qualification may have different attitudes towards using the internet and apps in clinical practice given that they could be in the role of using them when treating a patient. Thus given that 25% of participants were studying towards or had obtained a medical/health professional qualification we re-analysed the data pertaining to the attitudinal ratings by excluding these individuals. The pattern of results were identical to that obtained for the entire sample (i.e., a significant difference was obtained for all statements with the exception of the statement pertaining to students relying excessively on the internet / apps [data not shown]).
Some individuals may have security concerns in regards to using smartphones to conduct on-line banking which could be reflected in their behaviour in whether they use a smartphone to conduct on-line banking or not. Thus we divided participants who had smartphones into two groups, those that did and those that did not use a smartphone for on-line banking, to determine whether their levels of agreement to the statement pertaining to confidentiality in regards to doctors using apps (i.e., another activity that could pose security concerns) differed. No significant difference was found between participants who did (n = 55; M = 3.27; SD = 1.15) and did not (n = 61; M = 3.49; SD = 1.18) conduct on-line banking on smartphones in regards to their ratings for the statement pertaining to confidentiality and doctors using apps, t114 = 1.01, p = .313, two-tailed.
Discussion
All participants had internet access at home which reflects ABS data showing that a large number of individuals within Australia have access to the internet at home1. Furthermore, all participants owned a mobile phone with most of them having a smartphone. Thus a large portion of our participants had at least some familiarity with apps. However, only approximately one third of participants were aware that medical apps are available. It must be noted that we only asked participants if they knew of medical apps which are designed to be used by the general public (e.g., St John Ambulance Australia First Aid application) as opposed to apps designed for medical professionals (e.g., Medscape). Given that most participants were unaware of medical apps designed for the general public, it is even less likely that they would be aware of medical apps specifically designed for medical professionals.

Table 2. The number (with percentages in parentheses) of participants who rated strongly disagree, disagree, neither agree nor disagree, agree, and strongly agree for each statement regarding the use of the internet and mobile phone apps in clinical practice. Means, standard deviations and paired sample t-tests are reported were each level of agreement was assigned a number between 1 and 5 (i.e., 1 = strongly disagree; 5 = strongly agree).
All participants visited a medical facility at some point in their lives and the majority did so within the last 12 months (i.e., a time when the internet and apps were available). Thus most participants could potentially have observed a medical professional use the internet and/or apps. Not surprisingly, participants were more likely to have witnessed a medical professional use the internet than apps during consultations. This could possibly be attributed to medical professionals: 1) being more familiar with the internet than apps given that the internet preceded apps; 2) finding the use of a computer/desktop more professional to use than a smartphone; and 3) finding it easier to visually share information with patients on a computer screen than a small smartphone screen. Future studies will need to examine medical professional’s attitudes towards using the internet and apps in clinical practice.
In response to various statements pertaining to medical professionals using the internet and apps in clinical practice, participants’ mean attitudes for each statement tended to be close to the centre of the scale. When attitudes towards internet use were compared to that for app use it was found that participants were generally more accepting of medical professionals using the internet than apps. This could possibly be attributed to greater familiarity with the internet than apps given that the internet preceded apps.
The results showing no difference in confidentiality concerns in regards to medical professionals using apps to enter medical data between participants that did and did not use smartphones to conduct on-line banking were initially surprising. We anticipated that those who used smartphones for on-line banking would have less confidentiality concerns in regards to a medical professional entering medical data than those that did not use smartphones. The rationale behind this was that individuals who do not use their smartphones for on-line banking may have a general concern in regards to using such a device for anything that is confidential. Although using a smartphone for on-line banking and entering medical data both have a degree of confidentiality associated with them it must be acknowledged that these tasks are not completely analogous. For example, individuals have perceived control over their own on-line banking whereas they have no control in regards to a medical professional entering their medical data. Furthermore, the concept of entering medical data via a smartphone is likely to be new for most participants given that most have not witnessed medical professionals use apps in clinical practice. Thus irrespective of whether participants’ use smartphones for on-line banking or not, participants generally may have some degree of concern in regards to using smartphones for tasks they are unfamiliar with and where they lack control (e.g., entering medical data) which could explain our findings. Ideally we would have liked to conduct an analogous analysis regarding on-line banking via the internet and entering medical data via the internet but given that 92% of participants that had smartphones used the internet to conduct on-line banking this was not possible.
Limitations
Our study is restricted to individuals that have internet access and accessed it regularly. It is likely that individuals who lack internet access are less favourable of the concept of medical professionals using the internet during consultations than that reported here simply because they are less familiar with it.
Another limitation of our study is that 67% of participants were below 30 years of age and no participant was aged over 70 years. This is not surprising given that all participants had internet access at home and that age and internet use are likely to be related. However, it must be noted that ABS data show that internet use amongst individuals over the age of 60 years has substantially increased from 28% in 2003 to 47% in 200914. Thus over time the use of the internet may be taken up by a broader age range of individuals. Given that Australia’s population is aging15 and that elderly individuals are generally more likely to require medical attention than younger individuals it is important to ascertain elderly individuals’ attitudes towards the use of electronic devices (e.g., apps) within clinical practice. Therefore future studies should survey individuals that do not use the internet and / or are aged over 70 years to ascertain their attitudes towards medical professionals using the internet and apps in clinical practice.
Although our survey was targeted at the general public, it must be noted that some individuals who were studying towards or had obtained a medical/health professional qualification participated. It is unknown as to whether these individuals use electronic devices (e.g., apps) during clinical practice and consequently whether their attitudes are different to non-medical/health qualified individuals. However, when we re-analysed our data pertaining to the attitudinal ratings by excluding participants who were studying towards or had obtained a medical/health professional qualification we still found that mean responses were close to the mean of the scale and that participants’ attitudes were generally more favourable towards the internet than apps.
Conclusions
In conclusion, the general public was generally more accepting of the internet being used during clinical practice than apps. This finding could be attributed to greater familiarity with the internet as a direct consequence of it being available longer than apps. Perhaps the general public would be more accepting of app use over time once these smartphones have been available for a longer period of time and after they have witnessed medical professionals use them. These findings suggest that medical professionals intending to use electronic devices (e.g., apps) should clearly inform patients in regards to the intended purpose of using such a device and if applicable how information is stored prior to entering any patient data in order to potentially alleviate patients’ concerns. Repeatedly exposing patients to medical professionals using the internet and apps over time, in addition to adequately informing patients in regards to their intended use, may lead the general public to be more accepting of electronic devices being used in clinical practice in the future.
Acknowledgements
Dr Nicole Koehler was employed within the faculty of Medicine, Nursing and Health Sciences at Monash University at the time this study was conducted. We would like to thank Cai Feng Rachel Loh, a fifth year medical student at Monash University in 2012, for creating an on-line version of the survey which was designed by the authors, and Matthew Kang, a third year medical student at Monash University in 2012, for assisting with some of the descriptive statistical analyses.
References
1. Australian Bureau of Statistics, 2012, Household Use of Information Technology, Australia, 2010-11, cat. no. 8146.0, viewed 5 April 2012,
http://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/4E4D83E02F39FC32CA25796600152BF4?opendocument
2. Boulos, M. N. K., Wheeler, S., Tavares, C., & Jones, R. (2011). How smartphones are changing the face of mobile and participatory healthcare : An overview, with example from eCAALYX. Biomedical Engineering Online, 10, 24. 
3. Phillippi, J. C., & Wyatt, T. H. (2011). Smartphones in nursing education. Computers, Informatics, Nursing, 29, 449-454. 
4. Dasari, K. B., White, S. M., & Pateman, J. (2011). Survey of iPhone usage among anaesthetists in England. Anaesthesia, 66, 620–631.
5. Havelka, S. (2011). Mobile resources for nursing students and nursing faculty. Journal of Electronic Resources in Medical Libraries, 8, 194-199. 
6. Franko, O. I., & Tirrell, T. F. (2011). Smartphone app use among medical providers in ACGME training programs. Journal of Medical Systems [Online]. Available:
http://www.springerlink.com/content/p6t82ph541835u75/
7. Franko, O. I. (2011). Smartphone apps for orthopaedic surgeons. Clinical Orthopaedics and Related Research, 469, 2042–2048.
8. Bhanji, F., & Soar, J. (2011). Do smartphones help deliver high-quality resuscitation care? Resuscitation, 82, 1377-1378. 
9. Josephson, C. B., & Salman, R. A-S. (2010). Smartphones: Can an iPhone App help stroke physicians? The Lancet, 9, 765. 
10. Low, D., Clark, N., Soar, J., Padkin, A., Stoneham, A., Perkins, G. D., & Nolan, J. (2011). A randomised control trial to determine if use of the iResus application on a smart phone improves the performance of an advanced life support provider in a simulated medical emergency. Anaesthesia, 66, 255-262. 
11. Zanner, R., Wilhelm, D., Feussner, H., Schneider, G. (2007). Evaluation of M-AID, a first aid application for mobile phones, Resuscitation, 74, 487-494. 
12. Flannigan, C., & McAloon, J. (2011). Students prescribing emergency drug infusions utilising smartphones outperform consultants using BNFCs. Resuscitation, 82, 1424-1427. 
13. Koehler, N., Yao, K., Vujovic, O., & McMenamin, C. (2012). Medical students’ use of and attitudes towards medical applications. Journal of Mobile Technology in Medicine, 1:4, 16-21
14. Australian Bureau of Statistics, 2011, Age Matters, cat. no. 4914.0.55.001, viewed 5 April 2012, http://www.abs.gov.au/AUSSTATS/abs@.nsf/7d12b0f6763c78caca257061001cc588/ea6bbe44feac7fe2ca2572a400109d19!OpenDocument
15. Australian Bureau of Statistics, 2010, Population by Age and Sex, Australian States and Territories, cat. no. 3201.0, viewed 5 April 2012, http://www.abs.gov.au/ausstats/abs@.nsf/mf/3201.0
Read More