Posted on Feb 6, 2015 in News |
EyeXam is a vision screening app for iOS and Android devices that has recently been issued a patent from the U.S. Patent and Trademark Office. According to representatives from EyeXam, this makes it the first and only patented method for accurate self-guided mobile vision screening tests.
“We are excited to receive our patent for EyeXam and believe patent protection is timed perfectly in light of the explosion in mHealth apps. The ‘medicalized smartphone’ is impacting every aspect of health care, and eye care cannot lag behind,” says Dr. Nikki Iravani, founder and CEO of EyeXam.
The tests including visual acuity, colour vision, astigmatism and amsler grid have proved popular with consumers with the app downloaded more than 1 million times from the iTunes App store and Google Play to date. The app also allows patients to find a qualified eye care provider in their local area, exchange messages with the practice, schedule appointments, and search for eye-related information and articles using EyeWiki.
EyeXam asserts that the primary purpose of the app is to enable consumers to learn about their vision, understand the importance of professional eye examinations and connect with eye care providers.
The app is currently free to download on iTunes and Google Play.
By: Dr Joanne Teong
Source and image: www.eyexam.com
Posted on Feb 1, 2015 in Letter to the Editor |
Yulin Hswen, MPH1,2, Kasisomayajula Viswanath, PhD1,3
1Department of Social and Behavioral Sciences, Harvard School of Public Health, Boston, MA, USA; 2Center on Media and Child Health, Boston Children’s Hospital, Boston, MA, USA; 3Health Communication Core, Dana-Farber/Harvard Cancer Center, Boston, MA, USA
Corresponding Author: yhswen@gmail.com
Journal MTM 4:1:39–40, 2015
doi:10.7309/jmtm.4.1.9
In recent years, countless news stories, blog posts, and academic commentaries have highlighted the growing excitement surrounding the potential of mobile health (mHealth) technologies. Whether it is for treatment, diagnosis, illness monitoring or promoting healthy lifestyle behaviors, mHealth refers to the use of mobile and wireless devices such as smartphones or tablet computers for health or medical purposes, and as regularly illustrated in the Journal of Mobile Technology in Medicine, these emerging technologies offer innovative approaches to addressing complex medical and population health concerns.1,2 For example, leaders in medicine, government, and industry have championed mHealth as a strategy for treating acute and chronic illnesses, more efficiently conducting clinical and population-based health research, and addressing healthcare workforce shortages.3–5 In a recent commentary published in the Journal of the American Medical Association, Steinhubl and colleagues discussed the potential for emerging mobile technologies to transform health care.6 While we entirely agree that mHealth holds tremendous potential, we caution readers that these benefits may be differentially experienced across diverse groups, and may exacerbate as opposed to close health disparities.
The Internet revolution is a case in point. It was championed as a means to overcome socioeconomic, demographic and geographic barriers, yet considerable evidence shows a digital divide and fewer opportunities for disadvantaged individuals. It is possible that mHealth may be different given the rapid worldwide penetration of mobile telecommunication technologies; however, despite the decreasing costs of owning the actual devices, continuing access to data services through subscription represents a considerable expense for low-income individuals7 and limits access and use of these services.8 This creates challenges for many people to maintain a continuous and reliable wireless connection to the Internet, which would severely limit their ability to benefit from mHealth applications requiring continual illness monitoring, real-time data collection, or remote syncing to the virtual cloud. A recent survey conducted in the United States highlighted that expense was the single greatest barrier to owning a mobile device among a predominantly African American sample of low-income individuals with serious mental health concerns.9
Access, however, does not guarantee benefit from mHealth technologies. Difficult or unfamiliar user-interface may deter people from lower socioeconomic status to make effective use of mobile technologies for their health. Significant gaps in trust of health information from Internet sources has also been observed across low-income and ethnic groups.7 It is likely that such digital inequalities and lack of trust of health information may significantly limit the potential for mHealth to enable minority and low-income individuals to benefit through self-diagnosing acute symptoms, or tracking and managing chronic health conditions. This is of particular concern given the disproportionately elevated chronic disease burden impacting these individuals.10
Our aim is not to question the promise of mHealth, but rather to emphasize that just as stated by Steinbuhl and colleagues in their concluding remarks, “much remains to be done”.6 Just as clearly defined government regulations3, internationally recognized research guidelines11, and robust clinical trial evidence6 are critically necessary for advancing this nascent field, consideration of how mHealth technologies can be adapted and strategically delivered to address the needs of the most vulnerable low-income patients is of equal value. The role of mHealth technologies for addressing health disparities has received less attention12, though important opportunities exist. For instance, trends of increasing mobile phone penetration among low-income groups, evidence that at-risk minorities are more likely to search for health related information on their phones or on the Internet than mainstream populations, and the capacity to engage at-risk patients through greater personalization, facilitating social connections, or community outreach further support the promise of using these emerging technologies for reaching marginalized individuals.13,14
It is imperative that efforts to address health disparities through the elimination of health communication inequalities, targeted dissemination of culturally appropriate health information to at-risk minority groups10, or incentives programs aimed at addressing gaps in affordability and access to mobile health technologies7, must not be overshadowed by the hype or excitement of only the newest hi-tech devices. We sit at an exciting time where patients, researchers, clinicians, entrepreneurs and policy makers can shape how emerging mobile technologies will transform health care; let’s not squander this opportunity.
Disclosures
None for any author.
References
1. Perera C. The evolution of E-Health–mobile technology and mHealth. Journal of Mobile Technology in Medicine. 2012;1:1–2. 
2. Hswen Y, Murti V, Vormawor AA, Bhattacharjee R, Naslund JA. Virtual avatars, gaming, and social media: Designing a mobile health app to help children choose healthier food options. Journal of Mobile Technology in Medicine. 2013;2:8–14. 
3. Cortez NG, Cohen IG, Kesselheim AS. FDA regulation of mobile health technologies. New England Journal of Medicine. 2014;371:372–9. 
4. Collins F. How to fulfill the true promise of “mHealth”. Scientific American. 2012;307:16. 
5. Bartels SJ, Naslund JA. The underside of the silver tsunami—older adults and mental health care. New England Journal of Medicine. 2013;368:493–6. 
6. Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? Journal of the American Medical Association. 2013;310:2395–6. 
7. Viswanath K, Nagler RH, Bigman-Galimore CA, McCauley MP, Jung M, Ramanadhan S. The communications revolution and health inequalities in the 21st century: implications for cancer control. Cancer Epidemiology Biomarkers & Prevention. 2012;21:1701–8. 
8. Zickuhr K, Smith A. Digital differences. Pew Research Center’s Internet & American Life Project. 2012:1–41.
9. Ben-Zeev D, Davis KE, Kaiser S, Krzsos I, Drake RE. Mobile technologies among people with serious mental illness: opportunities for future services. Administration and Policy in Mental Health and Mental Health Services Research. 2013;40:340–3. 
10. Gibbons MC, Fleisher L, Slamon RE, Bass S, Kandadai V, Beck JR. Exploring the potential of Web 2.0 to address health disparities. Journal of Health Communication. 2011;16:77–89. 
11. Tomlinson M, Rotheram-Borus MJ, Swartz L, Tsai AC. Scaling up mHealth: where is the evidence? PLoS Medicine. 2013;10:e1001382. 
12. Horn IB, Mendoza FS. Reframing the disparities agenda: a time to rethink, a time to focus. Academic Pediatrics. 2013;14:115–6. 
13. Martin T. Assessing mHealth: opportunities and barriers to patient engagement. Journal of Health Care for the Poor and Underserved. 2012;23:935–41. 
14. Naslund JA, Grande SW, Aschbrenner KA, Elwyn G. Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube. PLoS One. 2014;9:e110171. 
Posted on Feb 1, 2015 in Featured |
![]()
The Editorial Board at the Journal of Mobile Technology in Medicine is proud to present Volume 4, Issue 1, the first issue of 2015. Mobile technology in Medicine is a rapidly developing area, and we hope to continue accelerating research in the field. We look forward to your submissions for Issue 2.
Posted on Jan 31, 2015 in Perspective Pieces |
Jennifer Franz-Vasdeki, PhD1, Beth Anne Pratt, PhD2, Martha Newsome, MPH3, Stefan Germann, PhD4
1Independent Consultant; 2Global Health Insights, LLC; 3World Vision International; 4World Vision International
Corresponding Author: Stefan_Germann@wvi.org
Journal MTM 4:1:35–38, 2014
doi:10.7309/jmtm.4.1.8
Introduction
The increasing availability and capacity of mobile devices is transforming accessibility and coverage in the health field. Globally, there are nearly 6 billion mobile cellular subscriptions with penetration reaching 80% in the developing world.1 Particularly in low and middle-income countries, the use of mobile telecommunication and multimedia technologies, known as mobile health or mHealth, can improve the quality of care and enhance efficiency of service delivery within healthcare systems. In particular, mHealth innovations offer tremendous opportunities to improve access to health-related information in hard to reach areas.2 Such opportunities include increased operational efficiencies, low cost delivery, as well as enhanced diagnosis, treatment and tracking of diseases.3 Like many resources and devices in the larger field of health informatics, mHealth solutions can also improve consumer access to and control over information they receive about health and can help to advance knowledge and skills while reducing complexity.4 mHealth tools can provide improved access to healthcare while creating cost efficiency and increasing capacity and quality of healthcare.5
Frontline health workers can benefit significantly from mHealth technologies, particularly in maternal and newborn health (MNH) as they can increase autonomy and improve motivation by facilitating and streamlining workloads and automating tedious duties.
Despite its demonstrated potential, mHealth tools and applications often struggle in practice. The mHealth landscape is comprised by a large number of pilot projects that are successful in one location, but do not make it to scale.5 This has lead to widespread scepticism of pilot projects and small-scale mHealth interventions in many parts of the world, particularly in low-income countries. In fact, the term ‘pilotitis’ has been coined in response to frequently expressed dissatisfaction from donors and governments about isolated mHealth interventions that are successful in one context, but not ‘rolled out’ due to a variety of technical, practical, economic and often institutional and political barriers.6–8
Initially, there was a distinct need for small-scale projects to gain a deeper understanding of technologies and applications. Likewise, not all mHealth projects are appropriate for scale; some serve a specific function or geographical area and are designed for the short-term. To integrate and build cross-sector partnerships around mHealth solutions, however, there is a growing need to coordinate activities and build an evidence base that allows for learning, communication, and understanding across sectors and contexts.
There is growing evidence to support the emergence of a new era in the mHealth evolutionary process with more and more successful mHealth intitiatives making it to scale and being rolled into national health schemes. Research around mHealth initiatives and their impact is evolving rapidly and the tracking of progress and success is increasing.9 The mHealth Alliance’s mHealth and MNCH: State of the Evidence report has found the increase remarkable and has called for even greater investment of resources in studying the effect mHealth interventions have on health outcomes, and emphasises the need to view gaps in the mHealth evidence as opportunities for future research.9
In particular, to make it out of the pilot phase, these initiatives require a number of key elements from the very beginning to ensure the possibility of scale. The mHealth Alliance has identified five key components that have increased the likelihood of a pilot project being mainstreamed into health systems, including: improved evidence, technology integration and interoperability, sustainable financing for mHealth, global and national policies that support the use of mHealth, and a health community that can design and deploy mobile technologies for health.9
Lemaire (2011) cites a number of complementary criteria required for overcoming ‘pilotitis’ and successfully scaling up of mHealth initiatives at national level. These criteria include:
- Building sustainability plans into mHealth initiatives from the point of planning;
- Ensuring that technological and logistical solutions to problems are locally feasible and appropriate;
- Securing buy-in from, and creating strategic partnerships with, key stakeholders, including national Ministries of Health, private sector mobile technology partners, technical agencies, local non-governmental organisations, and potential sources of financing whether private sector or donor-based;
- Aligning mHealth initiatives with local and national health priorities, and integrating initiatives into existing national- and sub-national health systems, structures, and policies;
- Putting in place data and interoperability standards so information fluidly feeds back into and informs national and sub-national health management information systems;
- Ensuring monitoring and evaluation is built into implementation plans, and provided with a sufficient budget.
The following case study offers a look at some of these basic ingredients and approaches that can help to achieve both scale and sustainability in the African context. We focus in particular on how closing persistent gaps increases the likelihood of mainstreaming mHealth initiatives into health systems.
Health Management Information Systems: mTrac
In 2012, following reports of an uncoordinated, ‘chaotic mushrooming’ of mHealth projects across the country, the Government of Uganda placed a moratorium on all mobile technology pilots until such time a coordinated set of technical standards and government strategies could be put in place.10 On the surface, the government’s declaration of a moratorium might suggest public sector mistrust in mHealth innovations. However, there have been a number of notable mHealth success stories in Uganda. One such success has been the government’s adoption and scale up of the mTrac platform for health information management. The Ugandan MoH was recognized by the African Development Bank for mTrac and it was rated one of the top ten eHealth projects of 2013.11
mTrac is a government initiative that originated as a pilot project within a Millennium Villages Project and Foundation for Innovative New Diagnostics (FIND). It was then handed over to the Government of Uganda for launch and scale up in December 2011. The Ministry of Health (MoH) fully owns and operates mTrac and it began to roll it out in four phases, each covering approximately twenty-eight districts.
mTrac is meant to be used as both an auditing and data collection tool. In particular, mTrac focuses on the collection, verification, accountability and analysis of data generated at community and health facility levels. With financial support primarily from the UK Department for International Development (DFiD), this is done in three key ways.12,13 Firstly, via SMS, in order to transmit weekly surveillance reports (i.e. information on disease outbreaks and stocks of anti-malarials) from health facilities to the MoH and District Health Offices (DHOs). Secondly, mTrac operates as an anonymous hotline providing a service delivery complaints toll-free number through which community members can report health service-related issues, including operating hours of health centres and stock outs of essential drugs in hospitals. Thirdly, through a mechanism known as ‘u-report’- where 235,000 registered stakeholders representing every community in Uganda collect regular feedback on developmental issues and engage elected representatives to discuss these issues.
mTrac is also available at the Village Health Team (VHT) level, feeding into the system information collected by community health workers. Data collected at this level includes information on malaria, severe malnutrition, and referrals to health facility, as well as on ACT and Amoxycillin stock.
mTrac was designed from the start to work within and through both the MoH’s existing software and paper systems of collection at the community and facility-level. By prioritising interoperability from the beginning, mTrac has aligned and integrated fully with the MoH and required limited additional investment in IT infrastructure or project implementation.
The MoH receives technical support from UNICEF and WHO, as well as financing from DfID, but mTrac is formally governed via a government-led Steering Committee chaired by the National Medical Stores, as well as via a dedicated eHealth Technical Working Group (TWG).13
The impact of mTrac is not yet known as it is still in its early stages. There is some evidence of low reporting rates by end users, and also weak health system responsiveness (e.g. supply chain inefficiencies mean that reports of drug stock outs cannot be acted upon).14 Such problems serve to highlight the fact that mHealth initiatives are not magic bullets, and their success is largely dependent on the strength of the health system into which they are introduced. Nevertheless, mTrac serves as a model for mHealth scale up as it focused, from the beginning, on a) designing interoperable systems that can be implemented to scale; b) aligning these systems into existing national structures, policies, and institutions; c) coordinating multiple public and private sector stakeholders, and leveraging their strengths; and d) focusing on minimising additional investment by government to ensure sustainability.
Conclusions
Achieving comprehensive health delivery systems supported by mHealth tools requires meaningful, productive communication across numerous sectors and stakeholders. Such stakeholders may include public health and healthcare delivery personnel, information technology and communication specialists, economists and finance professionals as well as evaluation and monitoring experts. Leadership is also needed from ministries, acting in concert, to provide the necessary guidance for innovators, companies, and organisations in order to develop meaningful mHealth tools targeted at national priorities. Patients or end users should also be included. There is a distinct need for engaging peers in the technology sector, thus requiring discussion to be extended to include stakeholders from across the full healthcare spectrum and along the full continuum of care.
Bringing mHealth solutions and interventions to scale requires cross-sector partnership brokering expertise, increased awareness, coordinated and directed financing, national and global policies to establish interoperability standards and data protection, and investment in the workforce to support long-term applications and initiatives.3 It also requires numerous and multi-sector stakeholders to be involved in national discussions to set strategies and operational plans to move forward in a unified fashion. The way forward needs to draw upon governments’ formal health sector development strategies and formal commerce, communications and related national strategies.
There remains limited evidence on the improved health outcomes generated from these projects. Better evidence would ensure improved coordination of activities to allow for learning, communication and thus understanding across sectors. For example, a project that demonstrates an increased quality of care or improved capacity of health care workers to manage patient load will provide the necessary evidence to funding organisations and national health systems that these projects are not only possible, but effective in changing delivery methods and improving efficiency, as well as generating tangible health benefits for the often most difficult to reach populations and doing so in a sustainable and affordable manner.
The mHealth field is currently dominated by people from the technology sector rather than health delivery practitioners. As mHealth is still in its nascent state, limited cross sector expertise is to be expected but has also been a contributor to ‘pilotitis’. Technologists can dazzle healthcare providers in the field or even policy makers with a new screen on a smartphone or a clever way to eliminate paperwork using SMS, however, this leads to a solution-based approach that does not consider long-term adaptability and sustainability implications. Once the technologist leaves, the pilot often falls apart because those in the field cannot support the application, or the technology/solution does not take into account the fact that the ‘solution’ needed to interoperate with some other equally important systems or processes.
As demonstrated with mTrac, there is a growing consensus among governments, funding bodies, and international organisations for the need of greater efforts in cross-sector partnerships to bring various stakeholders together. The Commission on Information and Accountability for Women’s and Children’s Health has called for 74 countries to have integrated the use of Information and Communication Technologies (ICT) in their national health information systems and infrastructure by 2015.15 The implementation plan of the Commission’s recommendation on use of ICT has three elements: develop a national mHealth plan, identify scalable projects, and build a knowledgebase of lessons learned and best practices.
Bringing mHealth solutions and interventions to scale requires numerous and multi-sector stakeholders to be involved in national discussions to set strategies and operational plans to move forward in a unified fashion. The way forward needs to draw upon government’s formal health sector development strategies and formal commerce, communications and related national strategies.
References
1. International Technical Union. The World in 2013: ICT Facts and Figures. (2013).
2. Chang, L. W. et al. Impact of a mHealth intervention for peer health workers on AIDS care in rural Uganda: a mixed methods evaluation of a clusterrandomized trial. AIDS and behavior 15, 1776–84, (2011). 
3. Mechael, P. N., Batavia, h., Kaonga, N., Searle, S., Kwan, A., Goldberger, A., Fu, L., Ossman, J,. Barriers and gaps affecting mHealth in low and middle income countries: Policy white paper. (mHealth Alliance and the Earth Institute, Columbia University, New York, 2010).
4. Ratzan, S. C. Connecting the MDGs and NCDs with digital health. Journal of health communication 16, 681–5, (2011). 
5. mHealth Alliance. Leveraging mobile technologies to promote maternal & newborn health: The current landscape & opportunities for advancement in lowresource settings. (The center for innovation & technology in public health; Public Health Institute, Oakland, CA, 2010).
6. Kuipers, P. et al. Collaborative review of pilot projects to inform policy: A methodological remedy for pilotitis? Australia and New Zealand health policy 5, 17, (2008). 
7. van Velthoven, M. H., Brusamento, S., Majeed, A. & Car, J. Scope and effectiveness of mobile phone messaging for HIV/AIDS care: a systematic review. Psychology, health & medicine 18, 182–202, (2013). 
8. Free, C. et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS medicine 10, e1001362, (2013). 
9. USAID. mHealth Compendium. (USAID, Washington DC, 2012).
10. New York Times. The Benefits of Mobile Health on Hold, <http://opinionator.blogs.nytimes.com/2013/03/13/the-benefits-of-mobile-health-on-hold/?_r=0> (2013).
11. Ugandan Ministry of Health. Health ministry initiative wins Africa e-health award. (http://www.mtrac.ug/mtrac-news, 2013).
12. DfID. Increasing Access to Antimalarial drugs in Uganda: Second Annual Review. (DfID, iati.dfid.gov.uk/iati_documents/4295929.doc, 2013).
13. Government of Uganda. Report on the mTrac National Launch. (Ministry of Health, Kampala, 2011).
14. Martyris, D. mHealth in Uganda. (mHealth Working Group, http://www.mhealthworkinggroup.org/resources/mhealth-uganda, 2013).
15. WHO. Keeping promises, measuring results: Commission on information and accountability for women’s and children’s health. (World Health Organization, Geneva, 2011).
Posted on Jan 31, 2015 in Original Article |
Yvonne O’ Connor, PhD1, John O’ Donoghue, PhD2
1Health Information Systems Research Centre, University College Cork, Cork, Ireland; 2Global eHealth Unit, Imperial College London, UK
Corresponding Author: y.oconnor@ucc.ie
Journal MTM 4:1:31–34, 2015
doi:10.7309/jmtm.4.1.7
On a global scale, healthcare practitioners are now beginning to move from traditional desktop-based computer technologies towards mobile computing environments1. Consequently, such environments have received immense attention from both academia and industry, in order to explore these promising opportunities, apparent limitations, and implications for both theory and practice2. The application of mobile IT within a medical context, referred to as mobile health or mHealth, has revolutionised the delivery of healthcare services as mobile technologies offer the potential of retrieving, modifying and entering patient-related data/information at the point-of-care. As a component of the larger health informatics domain mHealth may be referred as all portable computing devices (e.g. mobile phones, mobile clinical assistants and medical sensors) used in a healthcare context to support the delivery of healthcare services.
The usefulness of implementing IT in healthcare is reflected in current eHealth initiatives in resource-poor settings (e.g. Baobab Health in Malawi, M-Pedigree in Ghana, Nigeria and Kenya; Cell-Life in South Africa). In recent years attempts have being made to digitise WHO/UNICEF paper-based clinical guidelines when delivering paediatric healthcare services, namely: Integrated Management of Childhood Illness (IMCI) and Community Case Management (CCM). Both IMCI and CCM are stepwise and structured approaches, employed by Community Health Workers (CHW), towards reducing death, illness and disability while promoting improved growth and development among children under five years of age3,4. Digitising the IMCI and CCM guidelines offer profound opportunities to CHW (also referred to as Health Surveillance Assistants in Malawi, Africa) in terms of improving adherence to clinical guidelines, offering instant access to patient data independent of location and time and facilitating drug ordering via Short Message Service (SMS)5.
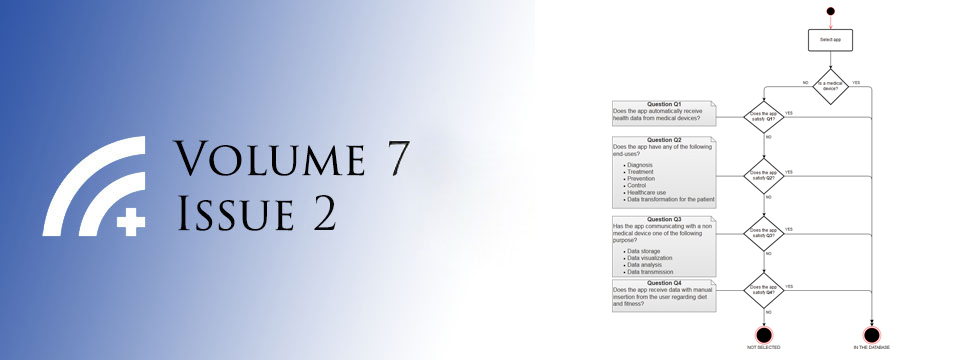
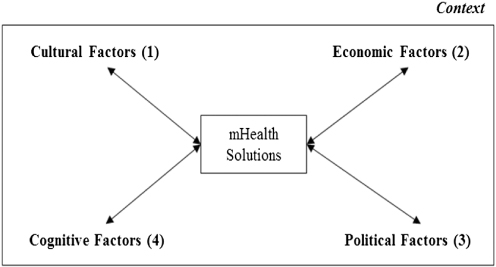
However, introducing mobile technology in a medical context within resource-poor communities is not without its challenges6. One obstacle faced by mHealth users is lack of user acceptance of the technology. Common factors which influence the decision making process of accepting mobile technology in medicine may include perceived usefulness, perceived ease-of-use of the technological tool7, performance expectancy, effort expectancy, social influence, facilitating conditions8. Arguably, the most imperative barrier faced by mHealth users in Africa is that of a contextual nature. The underlying premise behind this argument is that many mHealth solutions for use in developing countries are often developed in western societies. Such solutions have been criticised for failing to recognise the unique contextual factors associated with developing regions9. Contextual factors reflect external or driving elements that comprise the environment or conditions for decision making tasks10 and as a result, such factors can vary across populations and industries. Cultural, economic, political and cognitive dimensions are contextual factors which could influence how end users interact with mobile technology in medicine (referenced 1–4, Figure 1).
Figure 1: Contextual factors which should be incorporated into mHealth solutions
Cultural factors (1, Figure 1) denote a set of beliefs and norms that are both consciously and subconsciously held by any individual in the given society11. In the context of this paper, this refers to the principles/customs held by CHW in rural regions of Africa. Culture diversity between developing and developed countries can be observed based on “Individualism versus Collectivism”, “Power distance”, and “Masculinity versus Femininity”12. That is, developed countries such as Europe and U.S.A. are driven by individualist approaches whereas developing countries are concerned with collectivist strategies. Power distance reflects the way society distributes, shares, and enforces the power among its members13. Power holders in high power distance cultures such as Africa are much more comfortable with a larger status differential than low power distance cultures. Additionally, research in African countries shows preferential treatment towards males over females. It is worth noting, however, that cultural values cannot be easily adjusted to conform to any changes introduced by mHealth. This conformity, therefore, may have an impact on individual users’ intentions to adopt mHealth technologies in Africa. The authors suggest that ethnographic studies should be performed to capture local cultural dimensions similar to the work of Kitson (2011)14. In her work Kitson identified a number of cultural factors impacting the implementation of the Care2x hospital information system in Tanzania.
Economic factors (2, Figure 1) refer to the direct and indirect financial opportunities attributable to CHW in rural areas of developing regions. Without the necessary economic support for sufficient tools and resources, technology transfer from developed regions to Africa becomes very complicated, given the existing technological infrastructures at many African locations15. To help ensure that mHealth solutions are a viable option for African countries a cost analysis should be performed as advocated by Schweitzer and Synowiec (2012)16. Increased mobile coverage in rural areas, including faster network connectivity, is essential to realising the potential and scope of mHealth in developing countries. However, western societies should develop solutions that operate on commonly used mobile devices in developing regions. Many mHealth initiatives in Africa utilise the SMS functionality of mobile communication systems as a core connectivity method. The underlying rationale for using this low-cost functionality is that high-performance devices are not required to transmit data. For example, the effects of mobile phone SMS on antiretroviral treatment adherence in Kenya was examined17,18. These studies provide empirical evidence that mobile health initiatives can improve HIV treatment outcomes.
Political factors (3, Figure 1) refer to the governmental agenda of central administrations within developing regions. The planning and budgeting process in resource-poor areas are often constrained by expenditures in previous years. As a result, developing regions often face difficulty to mobilise funds for full-scale mHealth implementation as there may be no reliable or guaranteed governmental financial support for sustaining mHealth initiatives. If mobile technologies are to be successfully introduced across healthcare within developing regions, it is an essential that government agencies provide the necessary support, such as local Ministries of Health and local software industries to manage and maintain the software artefact. EHealth Nigeria is an example whereby an organisation collaborates closely with appropriate political powers to ensure the sustainability of Health Management Information Systems.
Cognitive factors (4, Figure 1) refer to users’ personal self-beliefs and opinions ability to interact with mobile technologies in a medical domain. That is, the degree to which a CHW perceives his or her ability to use mHealth technologies in the accomplishment of a task19. Cognitive dimensions do play an integral role in the use of mHealth technologies in developing countries as it is reported that such regions face education limitations (computer illiteracy) and a lack of English language skills. Research conducted in the health domain of Mozambique revealed that a limited amount of participants were computer literate, with only a minority of health workers at health facilities having the cognitive ability to interpret health data20. MHealth initiatives promoted by developed countries are often developed using the English language. This can hinder the use of mobile technology in medicine due to the lack of language translation abilities implemented within the software solution. It is therefore imperative that developers facilitate multi-language support to enhance the usability of mHealth technologies. Furthermore, training workshops should be provided to end users of mHealth solutions to enhance proficiency with the technology21. The importance of providing training workshops is reflected in the work performed by Baobab health in Malawi. They offer initial and refresher training courses to end users of their eHealth systems arguing that training is essential.
Conclusion
The status quo of the healthcare sector in Africa is plagued with uncertainty surrounding lack of resources (financial, technical and human), inadequate training to support health care providers, lack of technical infrastructure, limited participation in the development of medical/clinical standards, and lack of understanding of standards at national level)9. As a result, extant research on IT in the less-developed world has been severely limited. To add to this complexity IT solutions designed in developed countries have often failed to transfer effectively to African regions. To ensure that mHealth is a viable option for the health services sector in African countries many eHealth initiatives are attempting to address contextual factors as part of their development. This perspective piece argues that it is imperative for developers to encompass local cultural, economic, political and cognitive factors to ensure intentions, use and diffusion of mHealth initiatives.
Acknowledgements
“The Supporting LIFE project (305292) is funded by the Seventh Framework Programme for Research and Technological Development of the European Commission www.supportinglife.eu”
References
1. Wu J-H, Shu-Ching W, Li-Min L. Mobile computing acceptance factors in the healthcare industry: A structural equation model. International Journal of Medical Informatics 2007;76:66–77. 
2. Kjeldskov J, Skov M. Exploring context-awareness for ubiquitous computing in the healthcare domain. Personal and Ubiquitous Computing 2007;11:549–62. 
3. Handbook: IMCI management of childhood illness. 2005 edition. Geneva and New York, WHO and UNICEF, 2005. Available: http://whqlibdoc.who.int/publications/2005/9241546441.pdf
4. CORE Group, Save the Children, BASICS and MCHIP, 2nd Edition 2012. Community Case Management Essentials: Treating Common Childhood Illnesses in the Community. A Guide for Program Managers. Washington, D.C. Available: http://www.coregroup.org/storage/documents/CCM/CCMEssentialsGuide/ccmbook2012-online.pdf
5. Mitchell M, Getchell M, Nkaka M, Msellemu D, Van Esch J, Hedt-Gauthier B. Perceived improvement in integrated management of childhood illness implementation through use of mobile Technology: qualitative evidence from a pilot study in Tanzania. Journal of Health Communication 2012;17:118–27. 
6. Mechael PN. The case for mHealth in developing countries. Innovations 2009;4:103–18. 
7. Davis FD Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly 1989;13:319–40. 
8. Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Quarterly 2003;27:425–78.
9. Avgerou C. Information systems in developing countries: a critical research review. J Inf technol 2008;23:133–46. 
10. Fjerrnestad, J, Hiltz, SR. Experimental Studies Of Group Decision Support Systems: An Assessment Of Variables Studied And Methodology. In: Proceedings of the Thirtieth Hawaii International Conference on System Sciences, IEEE 1997: 45–65
11. Adler NJ. International Dimensions of Organizational Behavior. Cincinnati: South-Western College Publishing 2002.
12. Hofstede G. Culture’s Consequences: International Differences in Work-Related Values. Beverly Hills CA: Sage 1980.
13. Al-Abdul-Gader, AH. Managing Computer Based Information Systems In Developing Countries: A cultural perspective, IGI Global 1999.
14. Kitson N. A Convergence of Cultures and Strategies to Improve Electronic Health Record Implementation within a Tanzanian Clinical Environment. University of Alberta 2011.
15. Jimenez-Castellanos, A, de la Calle, G, Alonso-Calvo, R, Hussein, R, Maojo, V. Accessing advanced computational resources in Africa through cloud computing. 25th International Symposium on Computer-Based Medical Systems (CBMS), 2012: 1–4.
16. Schweitzer J, Synowiec C. The economics of eHealth and mHealth. Journal of Health Communication 2012;17:73–81. 
17. Lester, RT, Mills, EJ, Kariri, A, Ritvo, P, Chung, M, Jack, W, et al. “The HAART cell phone adherence trial (WelTel Kenya1): a randomized controlled trial protocol.” Trials 2009 Sep 22;10:87. 
18. Douglas G, Gadabu O, Joukes S, Mumba S, McKay M, Ben-Smith A, Jahn A, Schouten E, Lewis Z, van Oosterhout J. Using touchscreen electronic medical record systems to support and monitor national scale-up of antiretroviral therapy in Malawi. PLoS medicine 2010;7:e1000319. 
19. Compeau DR, Higgins CA. Computer self-efficacy: development of a measure and initial test. MIS Quarterly 1995;19:189–211. 
20. Braa J, Macome E, Mavimbe JC, Nhampossa JL, da Costa JL, Manave A, Sitói A. A study of the actual and potential usage of information and communication technology at district and provincial levels in mozambique with a focus on the health sector. The Electronic Journal of Information Systems in Developing Countries 2001;2:1–29.
21. Källander, K, Tibenderana, J, Akpogheneta, O, Strachan, D, Hill, Z, Ten Asbroek, AH, Conteh, L, Kirkwood, B, Meek, S. Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low-and middle-income countries: a review. J Med Internet Res 2013; 15: e17.
Posted on Jan 31, 2015 in Perspective Pieces |
Disha Kumar1,2, Monisha Arya, M.D., M.P.H3,4
1School of Social Sciences, Rice University, 6100 Main St., Houston, Texas 77005, U.S.A; 2Wiess School of Natural Sciences, Rice University, 6100 Main St., Houston, Texas 77005, U.S.A; 3Department of Medicine, Section of Infectious Diseases and Section of Health Services Research, Baylor College of Medicine, One Baylor Plaza, Houston, Texas 77030, U.S.A; 4Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center 2002 Holcombe Blvd (Mailstop 152), Houston, Texas 77030, U.S.A
Corresponding Author: disha.kumar@ricealumni.net
Journal MTM 4:1:25–30, 2015
doi:10.7309/jmtm.4.1.6
Low health literacy is a barrier for many patients in the U.S. Patients with low health literacy have poor communication with their physicians, and thus face worse health outcomes. Several government agencies have highlighted strategies for improving and overcoming low health literacy. Mobile phone technology could be leveraged to implement these strategies to improve communication between patients and their physicians. Text messaging, in particular, is a simple and interactive platform that may be ideal for patients with low health literacy. We provide an exemplar for improving patient-physician communication and increasing HIV testing through a text message intervention.