Posted on Apr 21, 2017 in Case report |
Wireless Smartphone Videography for Ocular Surgery SYSTEM
Jan-Bond Chan, MBBS, MMed Ophthal1,2, Embong Zunaina, MD, MMed Ophthal2, Ismail Shatriah, MD, MMed Ophthal2, Tajudin Liza-Sharmini, MBBS, MMed Ophthal2, Pik-Pin Goh, MD, MS Ophthal3
1Hospital Tuanku Ja’afar Seremban, Negeri Sembilan, Malaysia; 2Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia; 3Clinical Research Centre, Hospital Kuala Lumpur, Malaysia
Corresponding Author: janbond@hotmail.com
Journal MTM 6:1:1–4, 2017
doi:10.7309/jmtm.6.1.1
Purpose: To describe a self-made smartphone adaptor which can be attached to a surgical microscope and a smartphone telescope which can be wirelessly linked to an LED TV or monitor.
Methods: A smartphone slit lamp adaptor is built for microscope-assisted ocular surgery in which video can be recorded. For surgeries not utilising the microscope (such as those using surgical loupes), we employed a smartphone attached to a telescope for videography. Videos from both methods are then wirelessly streamed to a TV/monitor using EZCast, Google Chromecast or Apple TV.
Results: The video captured by a smartphone is comparable to conventional digital video recording. It is affordable, easy to use and highly portable.
Conclusion: Smartphone videography will be a valuable instrument in ophthalmology for both teaching and research purpose.
Posted on Oct 28, 2016 in News |
A team from Melbourne’s Centre for Eye Research Australia (CERA) has won this year’s Google Impact Challenge.
Medical doctor and PhD candidate Dr William Yan successfully pitched the team’s project, which uses a software algorithm to perform accurate, evidence-based visual acuity testing via webcam and Internet connection.
VisionAtHome’s aim is to help rural, remote and mobility-impaired users access and perform eye testing at home, particularly in areas with limited or no access to ophthalmologists. As Dr Yan explains, “94% of blindness or vision loss in Indigenous Australians is preventable or treatable. Less than 1% of eye specialists work in remote Australia, but almost all these areas have access to the Internet. Time is not on our side to bring changes in infrastructure to remote Australia, given its vastness, so telemedicine is a means of bridging the gap sooner.”

Dr William Yan, Project Lead of VisionAtHome. Photo: Centre for Eye Research Australia
CERA Principal investigator and Professor of Ophthalmic Epidemiology at the University of Melbourne, Professor Mingguang He was delighted with the outcome, describing VisionAtHome as a “simple hand-held solution for those who live far away from eye specialists. (It) has the potential to help millions of people not only in Australia but worldwide.“ This can expand to global areas of need beyond Australian communities, including the elderly, children, the physically disabled, and resource-poor settings in developing countries. In future, VisionAtHome aims to include Ishihara and visual field testing.
The Google Impact Challenge helps non-profits that use technology to solve social problems. The prize from Google will help CERA’s team translate their software to smartphone and mobile device applications, and undertake further research including clinical trials. For more information please visit cera.org.au.
By: Louise Teo
Posted on Jul 28, 2016 in Featured |
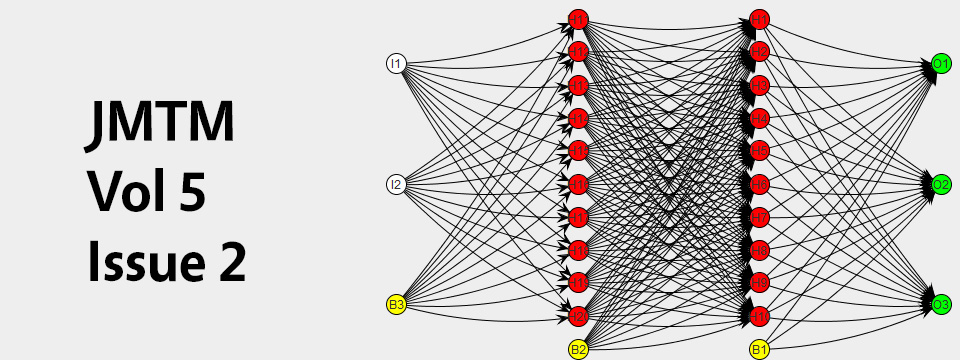
The Editorial Board at the Journal of Mobile Technology in Medicine is proud to present Volume 5, Issue 2. Mobile technology in Medicine is a rapidly developing area, and we hope to continue accelerating research in the field. We look forward to your submissions for Issue 3.
Posted on Jul 28, 2016 in Original Article |
María Luisa Zúñiga, PhD1, Kelly Collins, PhD2, Fátima Muñoz, MD, MPH2, Kathleen Moser, MD, MPH3, Gudelia Rangel, PhD4, Jazmine Cuevas-Mota, MPH2, Maureen Clark, BA2, Jose Luis Burgos, MD, MPH2, Richard S. Garfein, PhD, MPH2
1San Diego State University, School of Social Work, 5500 Campanile Drive, San Diego, CA, USA; 2Division of Global Public Health, Department of Medicine, University of California, San Diego, La Jolla, CA, USA; 3San Diego County Health and Human Services Agency, San Diego, CA, USA; 4Comisión de Salud Fronteriza, Sección México-Secretaria de Salud, Tijuana, Baja California, México
Corresponding Author: mlzuniga@mail.sdsu.edu
Journal MTM 5:2:12–23, 2016
doi:10.7309/jmtm.5.2.3
Background: Tuberculosis (TB) incidence in the U.S.-Mexico border region exceeds both countries’ national rates. The four U.S. states bordering Mexico account for nearly 40% of total U.S. TB cases. TB treatment monitoring using directly observed therapy (DOT) is a globally-accepted practice; however, it is resource intensive for providers and patients.
Aims: To determine whether Video DOT (VDOT)—a process whereby patients record themselves taking their medication by mobile phone and sending the videos to their TB care provider for observation—could be used to remotely monitor TB treatment adherence.
Methods: We conducted five focus groups with TB patients and four with TB care providers in San Diego, California, U.S. and Tijuana, B.C., Mexico.
Results: VDOT consistently received broad support: U.S. patients valued greater autonomy and Mexican patients valued improved privacy. Groups agreed technology would not be a barrier, but emphasized need for adequate patient training.
Conclusion: Patients and providers in both countries found VDOT conceptually feasible and acceptable.
Posted on Jul 28, 2016 in Original Article |
Julie B. Wang, PhD, MPH1,2,3, Janine K. Cataldo, RN, PhD3, Guadalupe X. Ayala, PhD, MPH2, Loki Natarajan, PhD1, Lisa A. Cadmus-Bertram, PhD4, Martha M. White, MS1, Hala Madanat, PhD2, Jeanne F. Nichols, PhD, FACSM5, John P. Pierce, PhD1
1Moores Cancer Center, University of California, San Diego, La Jolla, California, USA; 2Graduate School of Public Health, San Diego State University, San Diego, California, USA; 3Cardiovascular Research Institute, University of California, San Francisco, San Francisco, California, USA; 4Department of Kinesiology, University of Wisconsin-Madison, Madison, Wisconsin; 5Center for Wireless Population Health Systems, University of California, San Diego, La Jolla, California, USA
Corresponding Author: julie.wang@ucsf.edu
Journal MTM 5:2:2–11, 2016
doi:10.7309/jmtm.5.2.2
Background: As wearable sensors/devices become increasingly popular to promote physical activity (PA), research is needed to examine how and which components of these devices people use to increase their PA levels.
Aims: (1) To assess usability and level of engagement with the Fitbit One and daily SMS-based prompts in a 6-week PA intervention, and (2) to examine whether use/ level of engagement with specific intervention components were associated with PA change.
Methods: Data were analyzed from a randomized controlled trial that compared (1) a wearable sensor/ device (Fitbit One) plus SMS-based PA prompts, and (2) Fitbit One only, among overweight/obese adults (N=67). We calculated average scores from Likert-type response items that assessed usability and level of engagement with device features (e.g., tracker, website, mobile app, and SMS-based prompts), and assessed whether such factors were associated with change in steps/day (using Actigraph GT3X+).
Results: Participants reported the Fitbit One was easy to use and the tracker helped to be more active. Those who used the Fitbit mobile app (36%) vs. those who did not (64%) had an increase in steps at 6-week follow-up, even after adjusting for previous web/app use: +545 steps/ day (SE=265) vs. −28 steps/ day (SE=242) (p=.04).
Conclusions: Level of engagement with the Fitbit One, particularly the mobile app, was associated with increased steps. Mobile apps can instantly display summaries of PA performance and could optimize self-regulation to activate change. More research is needed to determine whether such modalities might be cost-effective in future intervention research and practice.
Posted on Jul 28, 2016 in Original Article |
Sora Park, PhD1, Sally Burford, PhD1, Leif Hanlen, PhD2, Paresh Dawda, MBBS/DRCOG3, Paul Dugdale, PhD/FAFPHM4, Christopher Nolan, MBBS/PhD5, John Burns, Adjunct Professor6
1News & Media Research Centre, University of Canberra, ACT, Australia; 2Data61, University of Canberra, Australian National University, ACT, Australia; 3Ochre Health Medical Centre, ACT, Australia; 4College of Medicine, Biology & Environment, Australian National University, ACT, Australia; 5College of Medicine, Biology & Environment, Australian National University, Canberra Hospital, ACT, Australia; 6University of Canberra, ACT, Australia
Corresponding Author: sora.park@canberra.edu.au
Journal MTM 5:2:24–32, 2016
doi: 10.7309/jmtm.5.2.4
Background: Ease of use, proximity to the user and various health maintenance applications enable mobile tablet devices to improve patient self-management. With mobile phones becoming prevalent, various mobile health (mHealth) programs have been devised, to improve patient care and strengthen healthcare systems.
Aims: This study explored how mHealth programs can be developed for type 2 diabetes patients through a co-design participatory workshop between practitioners and researchers. The aim was to design a mHealth pilot program from the input.
Methods: A co-design workshop was conducted with 15 participants, including general practitioners, specialists, nurses and a multidisciplinary research team. Participants generated 31 statements in response to a trigger question and engaged in a structured discussion. Thematic cluster analysis was conducted on the statements and discussions.
Results: Through the analysis, patients’ self-management and health system integration emerged as the main topics. Further analysis revealed that there were two distinct areas of patient self-management; ‘compelled’ and ‘empowered’.
Conclusion: With the results, a loose-knit mHealth pilot program was developed wherein patients with various levels of conditions and digital skills could be incorporated. In order to encourage sustainable changes, practitioners proposed that mobile devices must be situated in the patients’ everyday settings and that digital training should be provided.